When a pharmacist hands you a generic pill instead of your usual brand, most people assume it’s the same thing. But for NTI drugs, that assumption can be dangerous. Narrow Therapeutic Index drugs are a small group of medications where even tiny changes in dose or blood levels can lead to serious harm-think seizures, blood clots, or heart rhythm problems. And while the FDA says generics are safe to swap for these drugs, 27 states have passed laws that say otherwise. The result? A patchwork of rules that makes it harder for pharmacists, confusing for patients, and risky if you don’t know which state you’re in.
What Makes a Drug an NTI Drug?
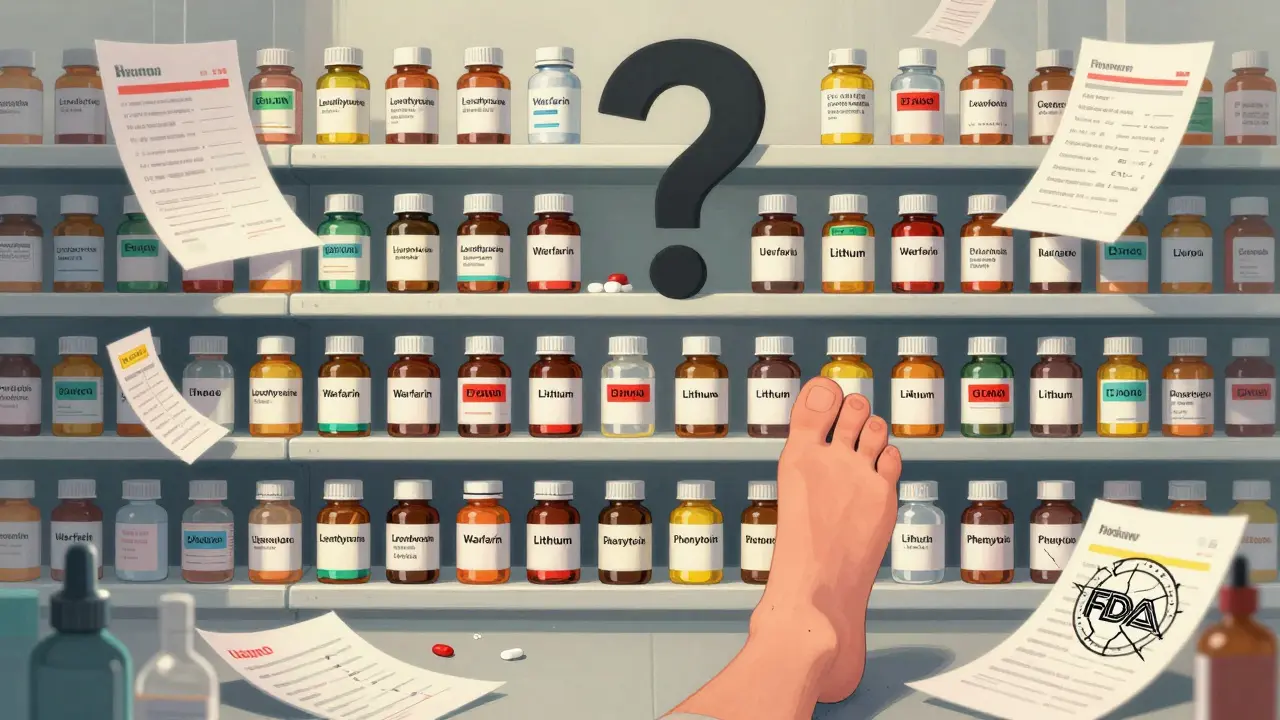
NTI stands for Narrow Therapeutic Index. These are drugs where the difference between a safe dose and a toxic one is razor-thin. A 5% change in blood concentration might mean the drug works perfectly-or it might trigger a life-threatening reaction. Common examples include warfarin (a blood thinner), levothyroxine (for thyroid issues), lithium (for bipolar disorder), and certain seizure medications like phenytoin and carbamazepine.
The FDA doesn’t officially label any drug as NTI in its Orange Book, which lists therapeutic equivalency ratings. But pharmacists and doctors know which ones to watch. The U.S. Pharmacist and other clinical sources have identified around 1,200 drugs as potential NTI candidates based on their pharmacology. These aren’t rare drugs-they’re used by millions. One study found that 32.4% of patients stabilized on brand-name levothyroxine saw their thyroid hormone levels shift after switching to a generic. That’s not a fluke. It’s a pattern.
Why Do States Step In When the FDA Doesn’t?
The FDA’s position has been consistent since 1997: the current bioequivalence standards-allowing generics to vary by up to 20% in absorption-are sufficient for all drugs, even NTIs. But clinicians and state regulators see it differently. At Harvard Medical School, Dr. Jerry Avorn pointed out that for drugs like levothyroxine, even a 5-10% variation can destabilize patients who are finely tuned. The American College of Clinical Pharmacy backed this up in 2023, citing 17 studies showing consistent shifts in blood levels after generic switches.
States aren’t ignoring science-they’re responding to real patient harm. A 2022 study in the Journal of the American Pharmacists Association found that states with NTI substitution restrictions saw an 18.7% drop in warfarin-related adverse events. That sounds small, but in real terms, it means fewer hospitalizations, fewer strokes, fewer deaths. For patients on these drugs, even a 0.3% absolute reduction matters.
How Do State Laws Differ?
There’s no national standard. Instead, you’ve got four main models:
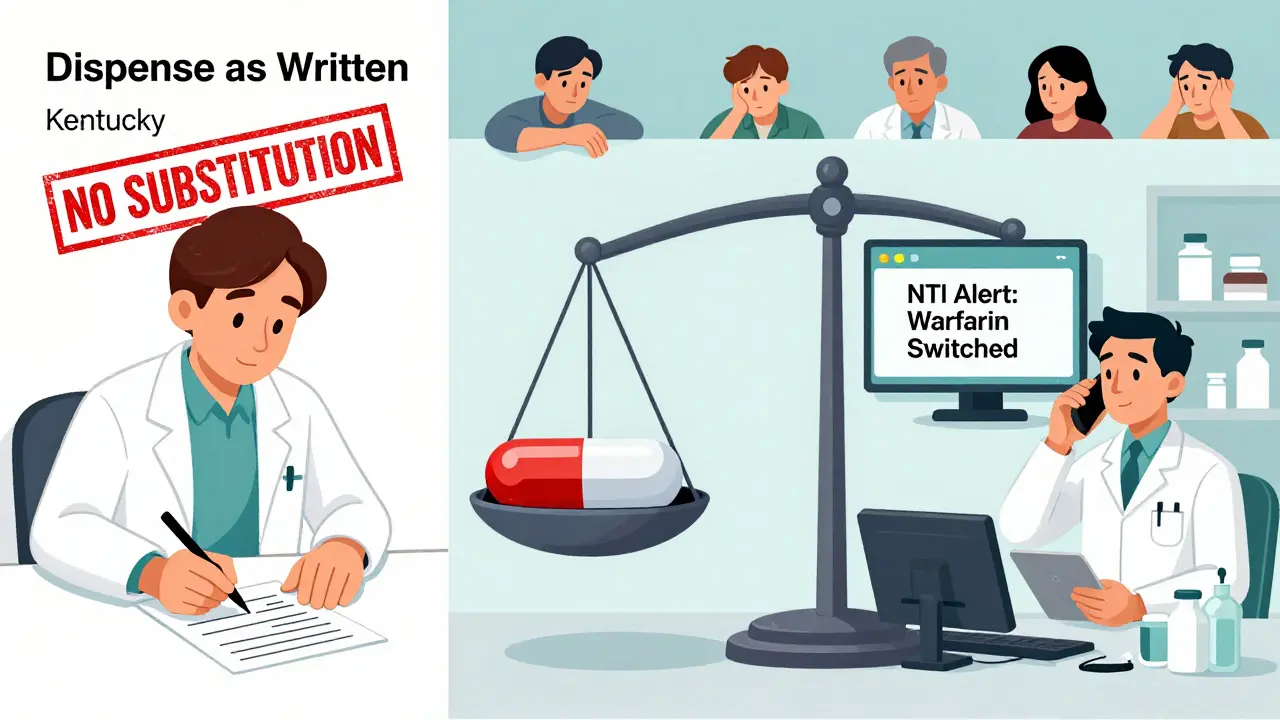
- Strict Prohibition Lists: Kentucky and Pennsylvania keep official lists of NTI drugs that can’t be substituted at all. That includes digitalis, warfarin, and antiepileptics. Pharmacists in those states must dispense the exact brand written on the prescription-or get a new one from the doctor.
- Recommendation-Based Rules: South Carolina doesn’t ban substitution outright. Instead, it recommends against swapping lithium, Premarin, Synthroid, insulin, and certain cardiac or asthma drugs. Pharmacists can still substitute-but they’re expected to know the risks and document their reasoning.
- Specific Exceptions: Tennessee allows generic substitution for most A-rated drugs, but makes one hard rule: no substitutions for antiepileptic drugs in patients with epilepsy. That’s a targeted, clinically focused approach.
- Notification Requirements: California doesn’t block substitution, but it forces pharmacists to notify the prescriber when switching any drug defined as having a “narrow therapeutic range,” where a 10% or less change in blood concentration could be dangerous. That’s a middle ground-preserving access to generics while keeping the prescriber in the loop.
Texas has its own twist: it bans substitution of anticonvulsants for epilepsy patients unless the doctor specifically authorizes it. That’s not about the drug class alone-it’s about the patient’s condition.
What This Means for Pharmacists
Imagine you’re a pharmacist working in a chain that spans three states. In Tennessee, you can swap a generic for a blood pressure pill-but not for an epilepsy drug. In Kentucky, you can’t swap warfarin at all. In California, you can swap it, but you have to call the doctor and log the change. One mistake, one missed rule, and you’re violating state law.
A 2023 survey by the National Community Pharmacists Association found that 68.3% of pharmacists who work across state lines get confused by these rules. Over 40% admitted they’d accidentally broken substitution laws in the past year. It’s not because they’re careless. It’s because the system is broken.
And it’s not just about NTI drugs. Forty-eight states have separate laws for biosimilar substitution-biologic drugs like insulin or Humira. Now pharmacists have to juggle two sets of rules, both evolving, both different. One pharmacist in a multistate chain told the American Journal of Managed Care: “I have to remember different rules for the same state, just because the store is in a different county.”
Why the FDA Won’t Change Its Mind
The FDA’s stance isn’t arbitrary. It’s based on decades of data showing that, on average, generics perform as well as brands. For most drugs, the 20% bioequivalence range is safe. But NTI drugs aren’t “most drugs.” They’re the outliers. The FDA argues that if a generic fails for an NTI drug, it’s a manufacturing issue-not a regulatory one. That’s true. But in practice, when a patient has a seizure after switching from brand to generic levothyroxine, the blame doesn’t go to the manufacturer. It goes to the pharmacist who filled it, the doctor who didn’t block the swap, and the system that let it happen.
Dr. John Jenkins, former head of the FDA’s drug review office, once said the agency’s position has been “sound and consistent.” But consistency doesn’t always mean safety. And patients aren’t asking for consistency-they’re asking for certainty.
What’s Changing in 2025?
Pressure is building. In September 2024, the FDA announced it would reconsider its position after the Senate Committee on Aging cited a Government Accountability Office report showing nearly 3,000 adverse events linked to NTI drug substitutions between 2019 and 2023. That’s not a rumor-it’s documented harm.
At the same time, the National Association of Boards of Pharmacy introduced the Model State NTI Substitution Act in January 2024. It proposes a single, evidence-based list of NTI drugs that all states could adopt. Twelve states have already introduced it as legislation. If it gains traction, we could see a major shift by 2027. IQVIA predicts 38 states will adopt standardized rules, cutting cross-state prescription errors by over 20%.
But there’s a trade-off. Standardization might reduce errors-but it could also reduce generic use. Right now, NTI restrictions block about 2.3% of potential generic substitutions. If more states follow suit, that number could grow. That means higher costs for patients and insurers. Express Scripts reported that NTI-related restrictions already increased their administrative costs by 5.7% compared to regular generics.
What Should You Do?
If you take an NTI drug:
- Ask your doctor to write “dispense as written” or “no substitution” on your prescription.
- Check your state’s pharmacy board website for its NTI drug list. Kentucky, Pennsylvania, and South Carolina all publish theirs online.
- Don’t assume your pharmacy will know the rules. If you’re in a new state, ask: “Is this drug on your substitution restriction list?”
- Monitor your symptoms. If you switch generics and feel different-fatigue, heart palpitations, mood swings, seizures-call your doctor immediately. Blood tests can catch changes before they become emergencies.
If you’re a pharmacist or work in healthcare:
- Keep a printed or digital copy of your state’s NTI rules. Update it every quarter.
- Use the FDA’s Orange Book-but don’t rely on it alone. It doesn’t mark NTI drugs. Your state’s list does.
- When in doubt, contact the prescriber. A quick call can prevent a crisis.
Frequently Asked Questions
Are all generic drugs unsafe for NTI medications?
No. Many patients switch safely between generics and brands for NTI drugs without issue. But the risk is higher than with other medications. A small percentage of people are sensitive to even minor changes in absorption. That’s why some states restrict substitution-not because generics are always dangerous, but because the consequences can be severe when they don’t work the same way.
Can a pharmacist refuse to substitute an NTI drug even if the state allows it?
Yes. Pharmacists have professional discretion. Even in states where substitution is permitted, a pharmacist can choose not to swap an NTI drug if they believe it’s unsafe for the patient. Many will call the prescriber to confirm, especially if the patient has a history of instability after a switch.
Do insurance companies block NTI substitutions?
Sometimes. Many insurers push for generics to save money, but they usually follow state law. If your state prohibits substitution for a certain NTI drug, the insurer can’t override that. However, in states that allow substitution, insurers may require prior authorization if you want to keep the brand-name version.
Is there a national list of NTI drugs I can check?
No. The FDA doesn’t maintain one. Some organizations, like the American Society of Health-System Pharmacists, publish unofficial lists based on clinical evidence, but these aren’t legally binding. Your only reliable source is your state’s board of pharmacy website.
What happens if I accidentally get the wrong version of my NTI drug?
If you notice a change in how you feel-mood swings, fatigue, irregular heartbeat, seizures-contact your doctor right away. Blood tests can quickly show if your drug levels are off. Most cases can be fixed by switching back, but delays can be dangerous. Keep your current prescription bottle and the new one to show your doctor the difference.
Next Steps
If you’re a patient on an NTI drug, make a plan: Know your drug, know your state’s rules, and talk to your pharmacist every time you refill. If you’re a provider, document your concerns clearly on prescriptions. If you’re a pharmacist, keep a checklist. This isn’t about resisting generics-it’s about making sure the right drug gets to the right person, every time.



I am from India and I never knew this was a problem. My mom takes levothyroxine and they switch generics here all the time. I will ask her doctor now.
Bro this is wild. NTI drugs are the bane of clinical pharmacists’ existence. You got 20% bioequivalence tolerance but for warfarin? That’s like playing Russian roulette with INR levels. The FDA’s stance is textbook but not bedside. Real patients aren’t averages. They’re people who crash when the pill color changes.
UK doesn’t have this mess. We use the BNF and trust the prescriber. If they want brand, they write it. Simple. No state-by-state chaos.
Oh here we go again with the ‘FDA is out of touch’ narrative. Let me guess - you’re the same person who thinks 5mg of lithium is the same as 5.1mg because ‘science says so’? Wake up. People are dying because some corporate pharmacist thinks ‘generic’ means ‘identical’. The FDA doesn’t care about your aunt’s seizure. They care about their quarterly profit reports.
they’re all in on this. the drug companies own the fda and the states. they want you to keep buying the expensive brand so they can keep raking in cash. you think this is about safety? no. it’s about control. they’ll let you die quietly while they bill your insurance for the brand name. i know people who died after switching. they called it ‘natural causes’
Thank you for laying this out with such clarity. As a pharmacist in Ohio, I’ve had to navigate this patchwork for years. I keep a laminated state-by-state cheat sheet taped to my counter. The real tragedy isn’t the legal complexity - it’s the patient who doesn’t know to ask. I always say: ‘If your drug changes color, ask if it’s the same.’ It’s not paranoia. It’s prevention.
There’s a quiet dignity in the way some states handle this - Tennessee’s epilepsy carve-out, California’s notification protocol. They’re not banning generics; they’re honoring clinical nuance. This isn’t anti-generic. It’s pro-patient. The FDA’s one-size-fits-all approach feels like treating a migraine with a sledgehammer. We need precision, not policy platitudes.
One must acknowledge the structural inefficiencies inherent in the current regulatory architecture. While the FDA's bioequivalence thresholds are statistically robust, they fail to account for inter-individual pharmacokinetic variability - particularly in populations with polypharmacy or hepatic impairment. The absence of a federally mandated NTI designation constitutes a critical governance lacuna. One might posit that harmonization through the NABP Model Act represents not merely a procedural improvement, but a moral imperative.
I used to work in a pharmacy in rural Georgia. One day, a 72-year-old woman came in crying because her new pills made her feel like she was floating. She was on levothyroxine. The generic was a different shape. She didn’t know it was switched. We called her doctor. She was in the ER by noon. I still think about her. We need to stop pretending this is just about cost. It’s about dignity. It’s about trust.
Oh wow. I can't believe you actually wrote this entire thing without mentioning that the FDA is being bought out by big pharma and the AMA is in on it. This is the exact same pattern as with insulin pricing. They want you to panic about substitution so they can charge you $500 for a 30-day supply of Synthroid. The real solution? Single-payer. Universal drug pricing. And a federal ban on all generic substitution for NTIs - period. No more state-by-state nonsense. Just let the government fix it before more people die.
I grew up in Ghana, where generics are the only option. We don’t have brand-name levothyroxine - only generics. And yet, people manage. Why? Because doctors monitor closely. Because labs are accessible. Because patients are educated. The problem isn’t the generic. It’s the lack of follow-up. In the U.S., we outsource care to pharmacists and then blame them when things go wrong. Fix the system - not the pill.