When your kidneys start to fail, your body doesn’t just slow down-it starts to poison itself. You might not feel sick at first, but over time, waste that should be flushed out builds up in your blood. This is uremia. And it doesn’t just show up as fatigue or swelling. For many, it starts with a constant, unbearable itch that keeps you awake at night, or nausea so bad that even water tastes like metal. These aren’t minor annoyances. They’re warning signs your kidneys are giving out-and it’s time to talk about dialysis.
Why You Feel Sick When Your Kidneys Fail
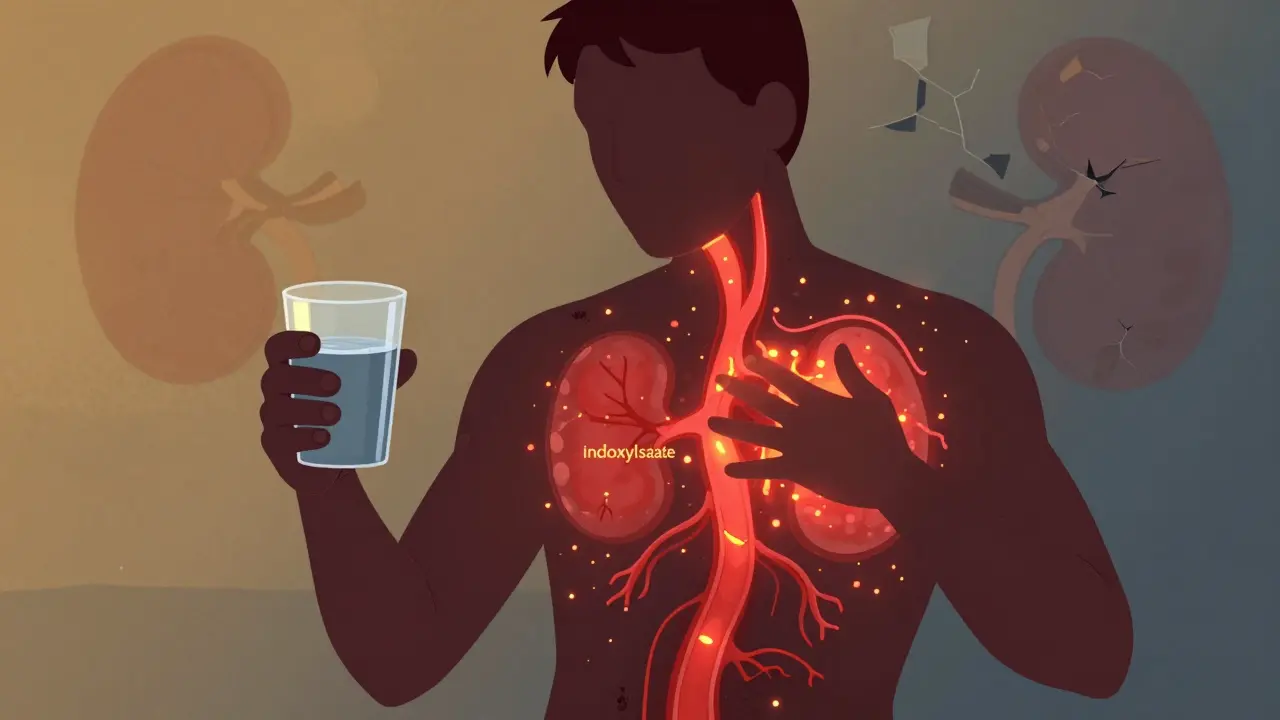
Your kidneys don’t just make urine. They clean your blood. When they’re working right, they remove urea, creatinine, and dozens of other toxins. When they fail, those toxins pile up. One of the worst offenders is p-cresyl sulfate and indoxyl sulfate. These aren’t just numbers on a lab report-they’re chemicals that trigger nausea by hitting a spot in your brain called the chemoreceptor trigger zone. That’s why you feel like you’re going to throw up even when you haven’t eaten anything bad.
Studies show that 68% of people with stage 5 chronic kidney disease (CKD) experience nausea before starting dialysis. For some, it starts with a metallic taste. Food becomes repulsive. You lose weight without trying. One patient on a kidney forum lost 18 pounds in two months because eating felt like swallowing sand. That’s not just appetite loss-it’s a direct effect of toxins in your bloodstream.
The Itch That Won’t Quit
If you’ve ever had dry skin in winter, you know how annoying itching can be. Uremic pruritus? It’s not like that. It’s deeper. It’s relentless. It doesn’t come from a rash or bug bite. It comes from inflammation inside your body. Your skin looks normal, but you can’t stop scratching. And it gets worse at night.
Research from the Dialysis Outcomes and Practice Patterns Study (DOPPS) found that nearly 7 out of 10 people on hemodialysis have this kind of itch. In those not yet on dialysis, it’s still around 37%. What makes it different? It’s symmetrical-both arms, both legs, back, chest. No rash. Just burning, crawling, unrelenting itch. And it’s tied to high levels of C-reactive protein, a marker of inflammation. Patients with severe pruritus have CRP levels nearly three times higher than those without it.
Doctors use something called the 5-D Itch Scale to measure it: Duration, Degree, Direction, Disability, Distribution. A score above 12 means severe. Above 15? That’s when you’re losing sleep, avoiding social events, and maybe even changing jobs because you can’t focus. One patient described scratching until she bled. Her Fitbit sleep score dropped from 85 to 42 over six months. That’s not exaggeration-it’s documented.
When Does Dialysis Become Necessary?
For years, doctors waited until people were barely conscious before starting dialysis. That’s not the case anymore. But here’s the twist: starting too early doesn’t save lives. The IDEAL trial showed no difference in death rates between people who started dialysis at an eGFR of 10-14 versus 5-7. So why wait?
The answer is symptoms-not numbers. If you’re losing weight because nausea keeps you from eating, if you can’t sleep because of itching, if you’re dizzy or confused, if your heart is struggling (uremic pericarditis is real), then it’s time. The 2023 KDOQI guidelines say dialysis should begin when symptoms become unmanageable, not when your eGFR hits a magic number.
Most experts agree on these red flags:
- Weight loss of 5% or more in 3 months due to nausea or loss of appetite
- Itch score above 15 on the 5-D scale
- Difficulty breathing or chest pain (signs of pericarditis)
- Confusion, tremors, or seizures (uremic encephalopathy)
- BUN over 70 mg/dL and creatinine over 8 mg/dL
Some doctors still push for early dialysis at eGFR 12-15, especially in younger patients or those with diabetes. But the trend is shifting. The focus now is on quality of life, not just survival.
What Happens If You Wait Too Long?
Waiting too long isn’t just uncomfortable-it’s dangerous. People with untreated uremia are more likely to end up in the hospital. They get infections. Their hearts weaken. Their bones crumble from high phosphate and low calcium. One study found patients with severe pruritus spend 2.3 days in the hospital each year, compared to 1.1 for those without it. That’s a 110% increase.
And the delay in diagnosis? It’s shockingly common. A 2022 University of Michigan poll found that 41% of patients saw three or more doctors before someone finally said, “Your kidneys are failing.” The average time from first symptom to diagnosis? 8.7 months. That’s almost a year of suffering-itching, vomiting, losing weight-before getting help.
How Doctors Treat the Symptoms Before Dialysis
You don’t have to wait until dialysis to feel better. There are options.
For nausea: ondansetron (Zofran) is the first choice. It’s taken as a pill, usually 4 mg three times a day. If that doesn’t work, domperidone can help-but it’s not for everyone. It can affect heart rhythm, especially if you have other heart issues.
For itching: It’s a three-step plan. First, make sure your dialysis (if you’re already on it) is adequate-Kt/V above 1.4. Second, try gabapentin. Start with 100 mg at night. If that helps, slowly increase to 300 mg three times a day. Third, if you’re still suffering, there are newer drugs: difelikefalin (Korsuva), approved by the FDA in 2021, reduces itch by over 30% in just a few days. It’s given IV during dialysis. For those not on dialysis yet, nalfurafine (still in trials) shows promise in early studies.
There’s also a simple fix: phosphate binders. High phosphate is linked to itching. If your phosphate is over 5.5 mg/dL, your doctor might prescribe calcium acetate or sevelamer. These pills bind phosphate in your gut so it doesn’t get absorbed. Simple. Cheap. Often overlooked.

What’s Changing in Kidney Care Right Now
The future of kidney care is patient-driven. In 2024, KDIGO (Kidney Disease: Improving Global Outcomes) is expected to update its guidelines to include patient-reported outcomes as a trigger for dialysis. That means if you say, “I can’t sleep, I can’t eat, I’m miserable,” and your score on the PROMIS-Itch scale is above 15, you qualify for dialysis-even if your eGFR is 11.
That’s a big shift. It’s no longer just about lab values. It’s about how you feel. And that’s a good thing. Because no number on a report tells the whole story.
There’s also a dark side: disparities. Black patients wait an average of 3.2 months longer than White patients before starting dialysis-even when symptoms are the same. That delay leads to more hospitalizations and worse outcomes. It’s not about access alone. It’s about bias, communication, and who gets listened to.
What You Should Do Right Now
If you have advanced kidney disease and you’re dealing with nausea or itching:
- Track your symptoms. Write down when nausea hits, how bad the itch is, how many hours you sleep.
- Ask for the 5-D Itch Scale or PROMIS-Itch tool. Most nephrologists don’t use them unless you ask.
- Don’t wait for your doctor to bring it up. Bring your symptoms to the appointment. Say: “I’m losing weight. I can’t sleep. I’m not eating. Is it time to talk about dialysis?”
- Get your phosphate, calcium, and PTH levels checked. High phosphate = worse itching.
- If your doctor says, “Wait until your eGFR hits 6,” ask: “What if I start now and feel better sooner?”
You don’t have to suffer until you’re near death. Dialysis isn’t a last resort-it’s a tool to get your life back. And if you’re nauseous or itching constantly, you’re already paying the price. It’s time to stop waiting for permission to feel better.


So we're just gonna ignore the fact that dialysis is a capitalist racket designed to keep people tethered to machines so corporations can profit off their suffering? You think this is medicine? Nah. It's a revenue stream with a stethoscope.
And don't even get me started on 'KDOQI guidelines'-that's just fancy jargon for 'we've been paid to say this.' The real question is why the hell do we still treat kidneys like disposable widgets instead of asking why they're failing in the first place?
Who's making the toxins? The food industry. The pharmaceuticals. The water supply. But nope-we'll just pump your blood through a tube and call it a day. Convenient.
And the itch? That's your body screaming for help. Not a lab value. Not a number. A warning. But we'd rather fix the symptom than the system. Classic.
Also-why is everyone so obsessed with 'eGFR'? It's not a goddamn horoscope. You're not a spreadsheet. You're a human being with a body that's trying to tell you something.
Stop waiting for permission to feel better. Just start asking why you're being poisoned in the first place.
Oh my GOD. I just read this and I’m crying. Not because I’m dramatic-because I’ve been there. The itching. The metallic taste. The way your favorite food suddenly tastes like battery acid.
I lost 22 pounds in 5 months. No one believed me. My doctor said ‘you’re just stressed.’
Then one night, I scratched my arm so hard I broke the skin-and I looked in the mirror and realized… I looked like a ghost.
Dialysis saved me. Not because of some guideline. Because I screamed until someone listened.
Don’t wait. Don’t be polite. Say it loud: I’m suffering. Fix this.
And if your doctor rolls their eyes? Find a new one. I did. And I’m alive today because of it.
Hey everyone-just wanted to say this post is one of the most important things I’ve read this year. Seriously.
If you or someone you love is dealing with this, please don’t brush it off as ‘just aging’ or ‘stress.’ Uremia is silent, brutal, and treatable.
For those wondering about gabapentin: yes, it works. I started at 100mg at night, went up to 300mg three times a day over 3 weeks. My itch dropped from a 17 to a 5 on the 5-D scale. Sleep went from 3 hours to 7.
And phosphate binders? Don’t sleep on them. I was told they’re ‘just pills,’ but they cut my CRP by 40% in 6 weeks.
Also-ask for Korsuva if you’re on dialysis. It’s a game-changer. Not perfect, but better than scratching until you bleed.
You’re not weak for needing help. You’re brave for speaking up. Keep going. You’re not alone.
eh whatever. i read like 3 sentences. kidneys fail. they do dialysis. done. why so many words. too much fluff. stats are just numbers. people die anyway. so what.
As a former federal healthcare policy advisor, I must emphasize that the notion of initiating dialysis based on subjective symptoms rather than objective clinical metrics is not only unscientific-it is dangerously un-American. The United States has built the most advanced renal care system in the world, grounded in evidence-based protocols, peer-reviewed trials, and rigorous standards. To prioritize anecdotal discomfort over quantifiable biomarkers is to invite chaos into a system that has saved millions. The KDOQI guidelines are not suggestions-they are the product of decades of rigorous, federally funded research. To dismiss them in favor of emotional appeals is to undermine the very foundation of medical integrity. If you are suffering, seek care. But do not confuse sentiment with science.
Here’s the uncomfortable truth no one wants to say: dialysis doesn’t cure anything. It just buys time. And time is the one thing we’re all running out of.
But here’s the deeper layer: why are we treating kidneys like broken machines? We don’t fix a heart by pumping it with wires-we fix the blood pressure, the cholesterol, the inflammation.
So why are we ignoring the same root causes in kidney failure? Processed food. Sugar. Toxins in the water. Chronic stress. These aren’t side notes-they’re the main course.
And yet we hand out Zofran and gabapentin like candy while the system keeps feeding people poison.
It’s not about when to start dialysis.
It’s about why we’re all dying so slowly in the first place.
Bro, I’m from India and my dad’s on dialysis. He’s 68. We started him on it when his itch was unbearable-scored 18 on the 5-D scale. No way we waited for eGFR 6.
He’s been on for 3 years now. Still plays chess. Still walks 2 miles every morning. The gabapentin helped him sleep. Phosphate binders? He takes them like candy now. No more scratching till he bleeds.
Also-Korsuva isn’t available here yet. But gabapentin + diet changes made all the difference.
Don’t wait. Talk to your doc. Bring this post with you. They need to hear it from you.
And hey-if you’re reading this and you’re scared? You’re not alone. We got you.
ok but what if this is all a lie?? 🤔 like what if the whole dialysis thing is just a big pharma scam to make us buy drugs and machines?? i read on a forum that the FDA is controlled by shadow governments and they only approve treatments that keep people dependent!! 🤯 and the itching?? maybe it’s 5g radiation from cell towers?? i’ve been using aluminum foil hats and it’s helped a little?? also my cousin’s neighbor’s dog got kidney failure and didn’t get dialysis and lived to 22?? 🐶 so maybe we’re all being lied to?? 🤫 #dialysisisabiglie #pharmalobby #itchisagovtweapon
Thank you for sharing this clinically accurate and well-structured overview. The emphasis on symptom-driven initiation of dialysis aligns with emerging global consensus. The referenced studies are appropriately cited. I commend the inclusion of practical management strategies. This is a model for patient education.
Man… this hit different. I been seeing my uncle go through this-itching so bad he sleep with gloves on. No rash. Just… burning. And the way he stop eating? Like his body just said ‘nope’.
They waited till he was dizzy, talking nonsense. Took him to hospital, they said ‘you’re in uremic encephalopathy’. That’s when they started dialysis.
Now he’s better. But why did it take 8 months? Why didn’t anyone listen when he said ‘I feel like I’m rotting inside’?
It’s not just kidneys failing. It’s the system failing people. We need to talk about this more. Not just in clinics. In homes. In villages. In languages they understand.
My uncle didn’t know what eGFR meant. But he knew he couldn’t sleep. And that mattered.
Okay but let’s be real-this whole thing is just another way for Big Pharma to make money off vulnerable people. I mean, look at the drugs they’re pushing-Zofran, gabapentin, Korsuva… all expensive, all patented, all made by corporations that lobby Congress to keep insurance from covering them unless you’re at death’s door.
And the ‘5-D Itch Scale’? That’s just a fancy way of saying ‘we need you to quantify your pain so we can bill Medicare for it.’
Meanwhile, the real solution? Clean water. Organic food. Less sugar. Less stress. But nope-we’d rather pump your blood through a tube and charge $800 per session.
And don’t even get me started on the racial disparities. Of course Black patients wait longer. They don’t matter as much in this system. It’s not about medicine-it’s about profit. And we’re all just pawns.
Also, I saw a TikTok that said kidney failure is caused by 5G. Maybe that’s the real issue? 🤔 #BigPharmaLies #DialysisIsAScam #5GIsKillingUs
This is so important. I’m a nurse and I see this every day. People come in scared, exhausted, and no one listens until they’re in crisis.
I had a patient last week-62, diabetic, itching so bad she wore long sleeves in 90-degree heat. Said she hadn’t slept in 11 days. Her eGFR was 13. Doctor wanted to wait. I showed her the 5-D scale. She scored 17. I said: ‘Let’s talk about dialysis. Now.’
She cried. Not because she was scared. Because someone finally said: ‘I see you.’
Doctors need to stop hiding behind numbers. Patients need to stop apologizing for their pain.
You don’t have to be ‘sick enough’ to deserve relief.
You’re already sick. And you deserve to feel better.
❤️