Procyclidine Blurred Vision Checker
This tool helps you determine if your blurred vision is likely related to your Procyclidine medication based on key symptoms and patterns.
Based on your answers, we'll provide guidance on next steps.
Ever taken a pill for Parkinson's and then noticed the world getting a little fuzzy? You’re not alone. Many people on Procyclidine blurred vision wonder why their eyesight suddenly feels off and what they can actually do about it. Below you’ll find the low‑down on what’s happening inside your eyes, why the drug can be the culprit, and practical steps you can take right now.
What is Procyclidine?
Procyclidine is an anticholinergic medication prescribed mainly to reduce tremors and rigidity in Parkinson’s disease and drug‑induced extrapyramidal symptoms. It works by blocking muscarinic acetylcholine receptors, which helps balance the dopamine‑acetylcholine mess in the brain. The drug has been on the market since the early 1970s and is still a go‑to for many neurologists.
How Procyclidine Works (and Why That Matters for Your Eyes)
When you block muscarinic receptors in the brain, you also affect similar receptors in other parts of the body. That includes the eye’s smooth muscles and the glands that produce tears. In technical terms, Muscarinic receptor a protein on cell surfaces that responds to the neurotransmitter acetylcholine helps control pupil size and the secretory function of the lacrimal gland.
Procyclidine’s anticholinergic action can therefore lead to a cascade of eye‑related changes: reduced tear production, difficulty focusing, and even temporary pupil dilation that skews vision.
Why It Can Blur Your Vision
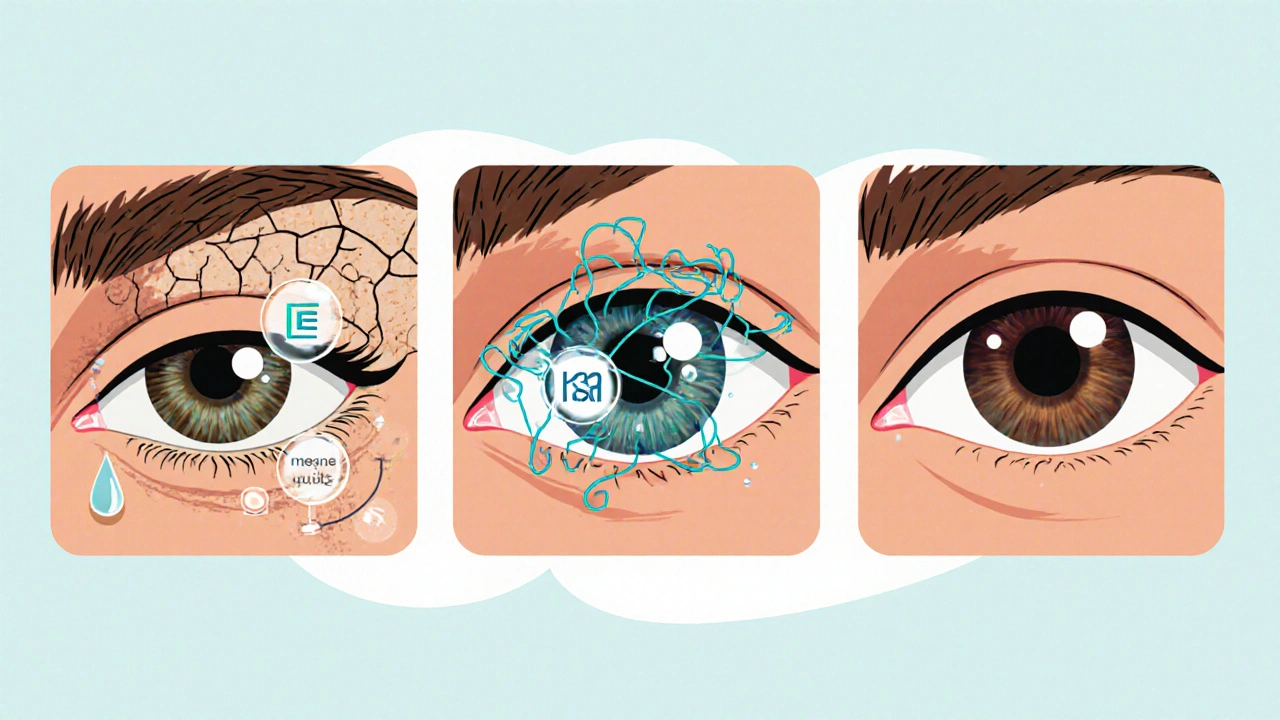
There are three main pathways that turn a helpful Parkinson’s pill into a blurry‑vision side effect:
- Dry eye syndrome: Less acetylcholine means the lacrimal glands release fewer tears, leaving the ocular surface dry and gritty.
- Accommodation fatigue: The ciliary muscle, which helps the eye focus on near objects, also relies on muscarinic signaling. Block that signal and your eyes struggle to switch focus, especially when reading or using screens.
- Pupil changes: Anticholinergics can cause mild dilation (mydriasis), reducing depth of field and making distant objects appear hazy.
All three can happen at once, and the effect feels like a foggy window over your world.
Common Eye‑Related Side Effects of Procyclidine
Besides the headline symptom of blurred vision, patients often report:
- Dry, itchy eyes (often labeled as Dry eyes a condition where insufficient tear fluid leads to irritation and visual discomfort)
- Photophobia - increased sensitivity to light
- Difficulty reading small print
- Eye strain after prolonged screen time
- Occasional double vision, especially at higher doses
Identifying Whether Procyclidine Is Behind Your Blurry Vision
The biggest challenge is separating drug‑induced blur from other common eye problems like refractive errors or cataracts. Here’s a quick checklist:
- Timing: Did the vision change start after you began or increase the dose of Procyclidine?
- Pattern: Is the blur worse when you’re reading, looking at a screen, or in bright light?
- Associated symptoms: Are you also experiencing dry or gritty eyes?
- Reversibility: Does the blur improve when you miss a dose (never skip without consulting a doctor, but an occasional missed dose can be informative)?
If you tick most of these boxes, the medication is likely playing a role.
Solutions and Management Strategies
Good news: most of the visual side effects are manageable, and many patients continue their Parkinson’s therapy without permanent damage.
| Cause | Solution |
|---|---|
| Reduced tear production | Artificial tears (preservative‑free), humidifier, omega‑3 supplements |
| Accommodation fatigue | Take breaks using the 20‑20‑20 rule, adjust screen font size, consider low‑dose pilocarpine eye drops under doctor supervision |
| Pupil dilation (mydriasis) | Wear sunglasses outdoors, avoid bright indoor lighting, discuss dose reduction with neurologist |
| General dryness & irritation | Stay hydrated, use a warm compress on eyelids, avoid smoke and windy environments |
Here’s a step‑by‑step plan you can try the next time you notice your vision slipping:
- Confirm the link: Note when the blur started and any dose changes.
- Start with lubricants: Use preservative‑free artificial tears four times a day for at least a week.
- Adjust your environment: Increase font size, enable dark mode on devices, and keep the room well‑lit but not glaring.
- Schedule a dose review: Call your neurologist. A 25‑30% dose cut or switching to a long‑acting formulation can often reduce eye side effects.
- Get an eye exam: A quick check with an ophthalmologist can rule out unrelated issues and may result in prescription lubricating ointments.

When to Seek Professional Eye Care
Most blur will improve with the tweaks above, but certain red‑flag symptoms warrant a prompt appointment:
- Sudden loss of vision in one eye
- Severe eye pain, especially behind the eye
- Persistent double vision that doesn’t improve after a few days
- Signs of infection: redness, discharge, fever
If any of these pop up, treat it like an emergency-go to a clinic or emergency department.
Preventive Tips for Long‑Term Users
Even if you’re not having problems now, a little foresight can keep your eyes sharp years down the line:
- Regular eye exams: At least once a year, even if you feel fine.
- Stay hydrated: Adequate fluid intake supports tear production.
- Balanced diet: Foods rich in omega‑3 fatty acids (salmon, chia seeds) and vitamin A (carrots, sweet potatoes) help maintain ocular health.
- Medication timing: Some patients find taking Procyclidine in the evening reduces daytime visual disturbances.
- Limit caffeine and alcohol: Both can worsen dry eye symptoms.
Frequently Asked Questions
Can Procyclidine cause permanent vision loss?
Permanent loss is extremely rare. Most visual side effects are reversible once the drug is adjusted or stopped. However, chronic dry eye can lead to surface damage if left untreated, so address symptoms early.
Is there a safer alternative for Parkinson’s tremor control?
Doctors sometimes switch to newer anticholinergic agents with fewer ocular side effects, like benztropine, or add a low‑dose dopamine agonist. Always discuss benefits and risks with your neurologist.
Do over‑the‑counter eye drops help?
Yes, preservative‑free artificial tears can relieve dryness and improve focus. Avoid drops with vasoconstrictors (like tetrahydrozoline) as they may worsen underlying dryness.
Should I stop Procyclidine if I notice blurred vision?
Never stop abruptly without medical guidance. Sudden withdrawal can cause rebound tremor or worsening Parkinson’s symptoms. Instead, arrange a dose review.
Are there lifestyle changes that can reduce the risk?
Staying hydrated, using a humidifier, limiting screen time, and protecting eyes from wind and bright light all help mitigate anticholinergic eye side effects.



Behold, the veil of clarity lifts only to be shrouded again-Procyclidine, the silent puppeteer of our sight, pulls the strings of tears and focus alike! In the theater of the brain, it whispers to the muscles, and the audience-our eyes-are left in a fog of existential doubt. Who among us has not gazed upon a screen, only to feel the world melt like butter in the sun? Yet, within this blur lies a lesson: even our pharmacologic allies can be double‑edged swords.
Understanding the mechanisms behind Procyclidine‑induced blurred vision empowers patients to take proactive steps. By adhering to the 20‑20‑20 rule, staying hydrated, and consulting an ophthalmologist, individuals can mitigate discomfort while maintaining essential Parkinson’s therapy. Consistency in using preservative‑free artificial tears and adjusting screen settings further supports ocular health. Let us embrace these strategies with confidence and optimism.
They don’t tell you that the pharma giants hide the full list of ocular side effects, so stay wary.
Sure, the drama is fun, but let’s not forget that many patients tolerate Procyclidine without any visual issues; the drug isn’t the villain in every story.
Artificial tears work well for most people, and taking short breaks from screens helps a lot.
Stop whining about a medication that’s been saving British patients for decades; if you can’t handle a little dryness, maybe you’re not cut out for this treatment.
Oh please! The global pharmaco‑industry is pulling the strings, and we’re left squinting in the dark while they profit-forget the “British” brag, it’s all a sick game!!!
It’s fascinating how a single anticholinergic can tip the balance of our visual world, quietly reshaping perception without a warning.
Indeed, embracing simple habits-like humidifiers and regular eye exams-can restore clarity, turning that silent shift into a story of triumph.
While some claim that eye drops solve the problem, the deeper issue may be the hidden agenda of drug trials that downplay long‑term ocular damage. Think about it: if the manufacturers truly cared, they’d fund independent studies, not just push us toward over‑the‑counter solutions. In any case, staying skeptical is healthier than blind compliance.
i think u should just stop using it and talk to your doc, thier might have an altnerative aint no need for all this theorizing.
Honestly, most of this is just hype-people can read a label.
First, keep a detailed log of when the blur starts and any dose changes, as this pattern often reveals the drug’s influence. Second, use preservative‑free artificial tears at least four times a day for a full week to assess improvement. Third, implement the 20‑20‑20 rule: every 20 minutes, look at something 20 feet away for 20 seconds, which eases accommodation fatigue. Fourth, increase screen font size and enable dark mode to reduce strain during prolonged use. Fifth, wear sunglasses with UV protection outdoors to counteract pupil dilation and photophobia. Sixth, stay well‑hydrated; adequate fluid intake supports natural tear production. Seventh, add omega‑3 rich foods such as salmon or chia seeds to your diet to promote ocular surface health. Eighth, consider a humidifier in dry environments, especially during winter heating. Ninth, discuss a possible dose reduction with your neurologist, as a 25‑30 % cut often lessens visual side effects without sacrificing tremor control. Tenth, ask about low‑dose pilocarpine eye drops under specialist supervision if accommodation remains an issue. Eleventh, schedule an annual comprehensive eye exam to rule out unrelated conditions like cataracts. Twelfth, avoid smoking and limit alcohol, both of which exacerbate dryness. Thirteenth, protect your eyes from wind and air conditioning drafts by using protective goggles when needed. Fourteenth, be vigilant for red‑flag symptoms such as sudden vision loss or severe eye pain and seek emergency care promptly. Finally, maintain open communication with both your neurologist and ophthalmologist to tailor a plan that preserves both motor function and visual clarity.