Myasthenia gravis isn’t just muscle weakness-it’s weakness that gets worse the more you use your muscles. Imagine lifting your eyelids only to have them drop again after a few seconds. Or struggling to chew food, then feeling fine after a nap. This isn’t laziness or fatigue from overwork. It’s myasthenia gravis (MG), a rare autoimmune condition where the body attacks the connection between nerves and muscles. The result? fatigable weakness-a hallmark that sets MG apart from almost every other neurological disorder.
How Myasthenia Gravis Breaks the Muscle-Nerve Connection
At the heart of MG is a breakdown at the neuromuscular junction. Normally, nerves release acetylcholine, a chemical that tells muscles to contract. In MG, the immune system produces antibodies that block or destroy the receptors for acetylcholine. Without those receptors, muscles don’t get the signal to move. And when they do move, they tire quickly because the signal keeps getting interrupted. About 80-90% of people with generalized MG have antibodies against the acetylcholine receptor (AChR). Another 5-8% have antibodies targeting muscle-specific kinase (MuSK), a different protein involved in nerve-muscle signaling. The rest are seronegative-no known antibodies found yet, but symptoms still match MG perfectly. This isn’t random. The disease tends to hit in two waves: early-onset (under 50), often linked to thymus gland changes like hyperplasia, and late-onset (over 50), where about 10-15% develop thymoma, a tumor in the thymus. The thymus, once thought to be just a leftover organ, is now known to be a key player in triggering the autoimmune response in MG.Fatigable Weakness: The Signature Symptom
You can’t diagnose MG by looking at someone at rest. You have to watch them move. The classic signs? Drooping eyelids (ptosis) and double vision (diplopia) in 85% of cases. These aren’t constant-they come and go. A person might wake up with clear vision, but by lunchtime, they’re squinting. Chewing becomes exhausting. Speaking turns into slurred words. Arms feel heavy lifting a coffee cup. Legs buckle after walking a few blocks. The key word is fatigable. Rest brings relief. A short nap can restore strength. That’s why many people go undiagnosed for years-they’re told they’re just tired, stressed, or anxious. But unlike regular fatigue, MG weakness follows a pattern: worse with activity, better with rest, predictable in its rhythm. Doctors use the Quantitative Myasthenia Gravis Score (QMGS) to measure severity. A score above 11 usually means the disease has moved beyond mild symptoms and needs more than just symptom control-it needs immunotherapy.First-Line Treatments: Symptom Control and Immunosuppression
Treatment starts with two goals: reduce symptoms fast and stop the immune system from attacking long-term. Pyridostigmine, an acetylcholinesterase inhibitor, is the first drug most patients get. It works by slowing down the breakdown of acetylcholine, giving more of it time to bind to the remaining receptors. Doses range from 60 to 240 mg daily, split into 3-4 doses. It helps-but it doesn’t fix the root problem. It’s like turning up the volume on a broken speaker. The signal’s still weak, but you hear it better. For real improvement, you need immunosuppression. Corticosteroids like prednisone are the go-to. Starting at 0.5-1.0 mg/kg per day, they suppress the immune system broadly. About 70-80% of patients see major improvement or even full remission. But side effects are real: weight gain, mood swings, bone loss, diabetes. Many patients gain 10-20 pounds within months. That’s why doctors don’t keep doses high forever. That’s where steroid-sparing agents come in. Azathioprine and mycophenolate mofetil are added early-usually within a month or two. Azathioprine takes 6-18 months to kick in but works in 60-70% of cases. Mycophenolate is faster, helping 50-60% of patients. Both reduce the need for steroids over time. But they come with their own risks: liver damage, nausea, increased infection risk.
Immunotherapy for Acute Crises and Refractory Cases
When MG flares up badly-when swallowing or breathing becomes dangerous-speed matters. That’s when IVIG (intravenous immunoglobulin) or plasma exchange (PLEX) are used. IVIG floods the bloodstream with healthy antibodies, which confuse the immune system and temporarily shut down the bad ones. It takes 5-7 days to work, and effects last 3-6 weeks. It’s safer, easier to give, and doesn’t require needles in large veins. PLEX, on the other hand, physically removes antibodies from the blood. It works faster-often within 2-3 days-and is preferred in severe cases like bulbar weakness or respiratory failure. But it needs a central line, carries infection risks, and requires hospital visits over several days. Both are equally effective in trials. The choice comes down to speed, access, and patient tolerance. In New Zealand, IVIG is more commonly used due to simpler logistics and fewer complications.Targeted Therapies: The New Era of MG Treatment
The last decade brought the biggest shift in MG treatment since corticosteroids. Rituximab, a drug that wipes out B-cells (the antibody factories), works wonders for MuSK-positive MG. Up to 89% of these patients reach minimal symptom status-far better than the 40-50% seen in AChR-positive cases. That’s why experts now test for MuSK antibodies early. If positive, rituximab might be the first immunotherapy, not a last resort. Then came efgartigimod, approved by the FDA in 2021. It’s not a broad immunosuppressant. It blocks the neonatal Fc receptor (nFcR), the body’s recycling system for IgG antibodies. By doing that, it causes a rapid drop-60-75%-in all IgG, including the bad ones. In the ADAPT trial, 68% of patients reached minimal manifestation status in just weeks. It’s given as a weekly IV for four weeks, then as needed. No hospitalization. No central line. Fewer side effects than steroids. Ravulizumab, approved in late 2023, targets the complement system-a part of the immune response that helps destroy muscle receptors. It’s given monthly by IV and shows promise for AChR-positive patients who haven’t responded to other treatments. These drugs aren’t cures, but they’re turning MG from a chronic, steroid-dependent disease into one that can be managed with precision.Thymectomy: Removing the Trigger
For patients aged 18-65 with AChR-positive generalized MG, removing the thymus gland (thymectomy) is now standard. The MGTX trial showed it nearly doubled the chance of reaching minimal manifestation status within three years compared to medication alone. About 35-45% of early-onset patients go into full remission after thymectomy and don’t need drugs anymore. The surgery isn’t risky-it’s usually done laparoscopically. Recovery takes a few weeks. But the payoff? Freedom from daily pills, fewer infections, no more steroid weight gain.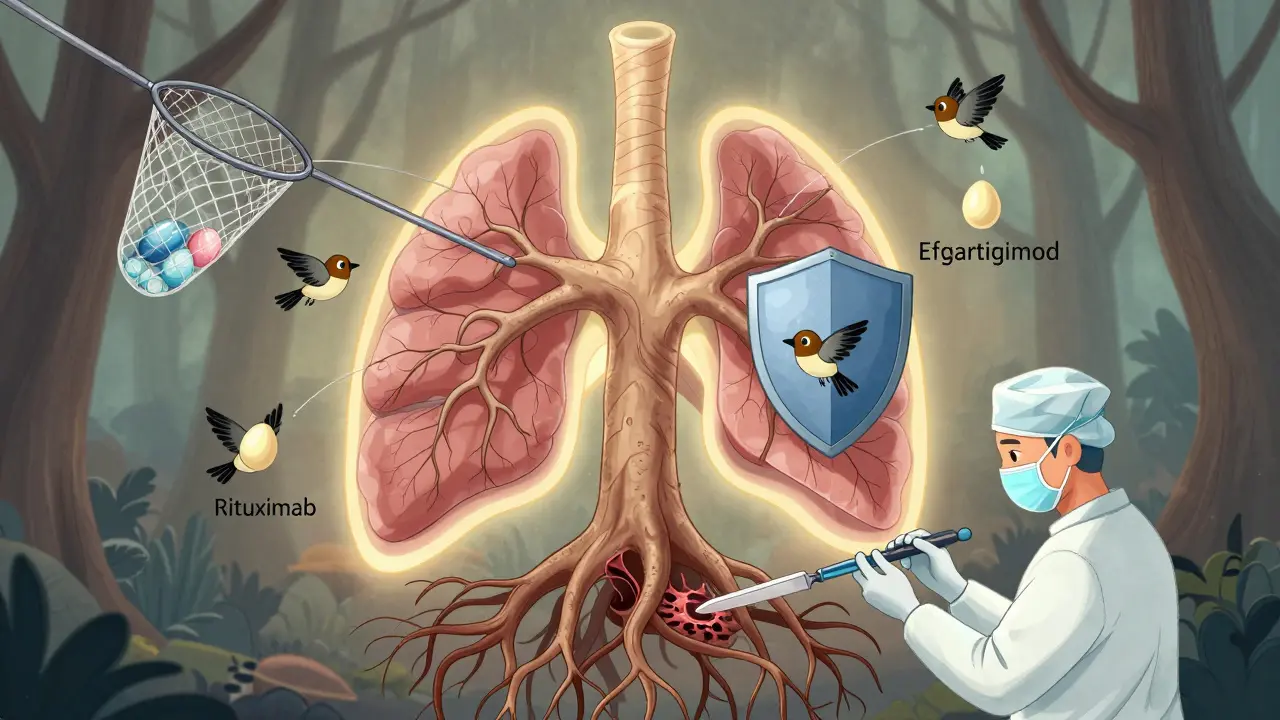
What Doesn’t Work-and What Can Make Things Worse
Not all treatments are equal. Some can actually harm. Immune checkpoint inhibitors (ICIs), used to treat cancers like melanoma and lung cancer, can trigger severe MG-or make existing MG explode. In one study, 60% of patients who developed ICI-induced MG also had heart inflammation (myocarditis). Eighty-three percent needed ICU care. If someone with MG gets cancer, oncologists must be warned. The risk isn’t theoretical-it’s deadly. Also, some antibiotics (like macrolides and fluoroquinolones), beta-blockers, and even magnesium can worsen MG symptoms. Always check with a neurologist before starting any new medication.Living with MG: Long-Term Realities
Most people with MG need long-term treatment. About 85-90% require ongoing immunosuppression. But that doesn’t mean a life on the sidelines. Many reach minimal manifestation status-meaning symptoms are so mild they barely affect daily life. A 2023 study showed that with proper treatment, 90% of patients can work, drive, and travel normally. The biggest challenge? Tapering. Doctors want to reduce drugs to avoid side effects. But if you taper too fast-before 2 years of stable symptoms-there’s a 40-50% chance of relapse. Patience is part of the treatment. And while MG can’t be cured yet, it can be controlled. With the right mix of targeted immunotherapy, careful monitoring, and lifestyle adjustments, most people live full, active lives.What’s Next for MG Treatment?
The future is focused on stopping the disease before it starts. Researchers are testing drugs that target specific B-cell types, block cytokines like IL-6, or silence autoantibody production without broad immune suppression. Rozanolixizumab, a subcutaneous nFcR blocker, is in phase 3 trials. It could be given at home like insulin. Inebilizumab, which targets a different B-cell marker, is also showing promise. The Myasthenia Gravis Foundation’s 2023 roadmap says the top goal is disease modification without chronic immunosuppression. In other words: fix the immune system’s mistake, not just cover it up. For now, the tools we have-pyridostigmine, steroids, rituximab, efgartigimod, thymectomy-are better than ever. The goal isn’t just survival. It’s living without weakness.Is myasthenia gravis curable?
There’s no cure yet, but many people achieve long-term remission-especially after thymectomy or with targeted immunotherapies. About 35-45% of early-onset AChR-positive patients stop needing medication after surgery. Others reach minimal manifestation status, where symptoms are so mild they don’t interfere with daily life.
Can stress make myasthenia gravis worse?
Yes. Stress, infections, and extreme temperatures can trigger flare-ups by activating the immune system. That’s why managing stress, avoiding illness, and staying cool in hot weather are part of daily care. It’s not the stress itself causing weakness-it’s how it pushes your immune system into overdrive.
Do all MG patients need immunotherapy?
Not immediately. People with mild, eye-only symptoms (ocular MG) may only need pyridostigmine and close monitoring. But if weakness spreads to the face, throat, or limbs-usually within two years-immunotherapy is almost always needed. About 85-90% of patients end up on some form of immunosuppression long-term.
How do I know if my treatment is working?
Your doctor will track your symptoms and use the Quantitative Myasthenia Gravis Score (QMGS). A drop of 5+ points means improvement. More importantly, you’ll notice real changes: less eyelid drooping, easier swallowing, more energy after activity. If you’re not improving after 6-12 months on a drug, it’s time to adjust.
Can I get pregnant with myasthenia gravis?
Yes, but it requires careful planning. Pregnancy can worsen MG in the first trimester and improve later. Some medications, like mycophenolate, are unsafe during pregnancy-others, like azathioprine and pyridostigmine, are considered safe. Work with a neurologist and obstetrician before conceiving. Most women with well-controlled MG have healthy pregnancies and babies.
Are there natural remedies or supplements that help?
No supplements or diets have been proven to treat MG. Some people take vitamin D or omega-3s for general immune support, but they don’t replace medication. Avoid herbs like echinacea or astragalus-they can stimulate the immune system and make MG worse. Always talk to your doctor before trying anything new.
What should I do if I suddenly can’t breathe or swallow?
This is a medical emergency called a myasthenic crisis. Call emergency services immediately. Do not wait. Go to the hospital. You may need IVIG, plasma exchange, or mechanical ventilation. Delaying treatment can be life-threatening. Keep an emergency plan ready-give a copy to family, friends, and your doctor.



This post is basically a pharmaceutical ad disguised as medical education. They’re pushing these expensive biologics like efgartigimod and ravulizumab like they’re miracle cures, but have you seen the price tags? And don’t get me started on how they gloss over how steroids wreck your body. This isn’t medicine-it’s profit-driven propaganda. Patients are being sold hope while their insurance denies them the basics. Wake up, people.
And thymectomy? Sure, it works for some. But who’s paying for the surgery? Who’s covering the time off work? The system doesn’t care about your quality of life-it cares about billing codes.
I’ve seen patients die because they couldn’t afford IVIG. And now we’re celebrating ‘targeted therapies’ like they’re heroes? No. They’re luxuries. And the real tragedy is that most people with MG will never see them.
Stop glorifying Big Pharma’s latest toys. Fix the system first. Then we can talk about ‘precision medicine.’
Weakness that improves with rest is the key. Not fatigue. Not laziness. Not depression. That’s the distinction. Everything else is noise.
They never mention the real cause. The thymus isn’t just ‘involved’-it’s being manipulated. You think all these autoimmune cases popped up out of nowhere? Think again. Fluoride in the water. EMF from 5G. Vaccines altering immune memory. The thymus is the first target. They know it. They’ve known it for decades.
Why do you think MG spikes in military veterans? Why do so many cases follow a flu shot? They’re testing something. And you’re the lab rat.
They want you dependent on IVIG and biologics. That’s the endgame. Control the immune system, control the patient. And the government? They’re in on it. Look at the FDA approvals-timing is too perfect. Coincidence? I don’t think so.
ok so i just read this and like… i think my cousin might have this?? she’s always tired and her eyelids droop but she says it’s just ‘stress’ and she’s been seeing therapists for years. i’m gonna send her this. also, no, echinacea is not a cure lol. i tried it. made my face swell. 🤮
Thank you for writing this with so much care 💙
My aunt was misdiagnosed for 5 years before they found out it was MG-she thought she was just getting old. Now she’s on pyridostigmine and it’s changed everything. She can hold her grandkids again.
It’s so hard when doctors don’t know this disease. I’m so glad someone’s explaining it clearly. I’ll share this with every neurology office in my city. We need more of this.
Also-yes to thymectomy. My aunt had it last year and she cried when she realized she didn’t need steroids anymore. That’s freedom.
And no, vitamin D won’t fix it. But it helps your bones. So take it. Just don’t expect it to save you 😊
I appreciate the depth of this post-truly, it’s one of the most comprehensive summaries I’ve seen on MG in a non-academic space.
But I do wish there was more on the psychological toll: the guilt of needing help, the shame of canceling plans because your voice gave out, the isolation of being told ‘you look fine’ when you feel like you’re dissolving.
And while the drugs are important, the real breakthrough is community. The online MG groups-where people trade tips on how to button shirts with weak fingers, or how to explain to your boss that ‘rest’ isn’t laziness, it’s survival.
Medicine treats the body. But we need to treat the soul too.
Thank you for seeing us.
Let us not conflate pathophysiological mechanisms with therapeutic efficacy. The neuromuscular junction is not merely a synapse-it is an ontological battleground where molecular mimicry, epitope spreading, and thymic dysregulation converge in a symphony of autoimmunity.
One must interrogate the epistemological foundations of the QMGS: is it truly a valid instrument, or merely a reification of clinical bias under the guise of quantification?
Furthermore, the privileging of biologics over holistic immunomodulation reveals a paradigmatic myopia-a reductionist fetishization of pharmacological intervention that neglects the embodied phenomenology of fatigue.
Perhaps, instead of targeting nFcR, we ought to interrogate the sociopolitical architecture of healthcare access that renders these therapies inaccessible to 92% of the global population.
Thus, while your post is empirically sound, it remains epistemologically colonial. A true cure lies not in antibody blockade, but in epistemic justice.
Everyone’s talking about these new drugs like they’re magic, but the truth is most people with MG never even get to try them. I’ve seen guys in India who can’t afford pyridostigmine, let alone IVIG. And here we are, celebrating FDA-approved biologics like it’s some kind of victory. What about the rest of the world? You think a guy in Lagos has access to efgartigimod? Please. The whole conversation is built on privilege.
And thymectomy? Sure, it works if you’re young, white, and have insurance. But what about the 70-year-old with diabetes and no Medicaid? They just get told to ‘rest more.’
Stop pretending this is about science. It’s about money. And the people who need help the most? They’re still waiting.
Why is the U.S. letting Big Pharma control our healthcare? We pay more for these drugs than any other country. Why can’t we just make these treatments affordable? Why does it take 10 years to approve a new drug when the science is already there?
And why are we letting foreign companies patent everything? The U.S. invented most of this. We should be manufacturing efgartigimod here, not shipping it overseas for profit.
Thymectomy? Great. But why isn’t it covered by Medicare like a knee replacement? Why are we treating a neurological disease like a luxury?
It’s time we stop letting corporations decide who lives and who suffers. This isn’t healthcare. It’s a rigged game.
I just want to say thank you to everyone who shared their stories here. I’m a nurse who works with MG patients, and I see how hard this is-not just for them, but for their families too.
One of my patients, a single mom, told me she used to cry after her kids went to bed because she couldn’t lift them anymore. Now she’s on mycophenolate and she’s back to reading them bedtime stories.
This disease is invisible, but your strength isn’t. Keep speaking up. Keep asking for help. And if you’re reading this and you’re scared? You’re not alone.
I’m here. We’re here.
You’ve got this.