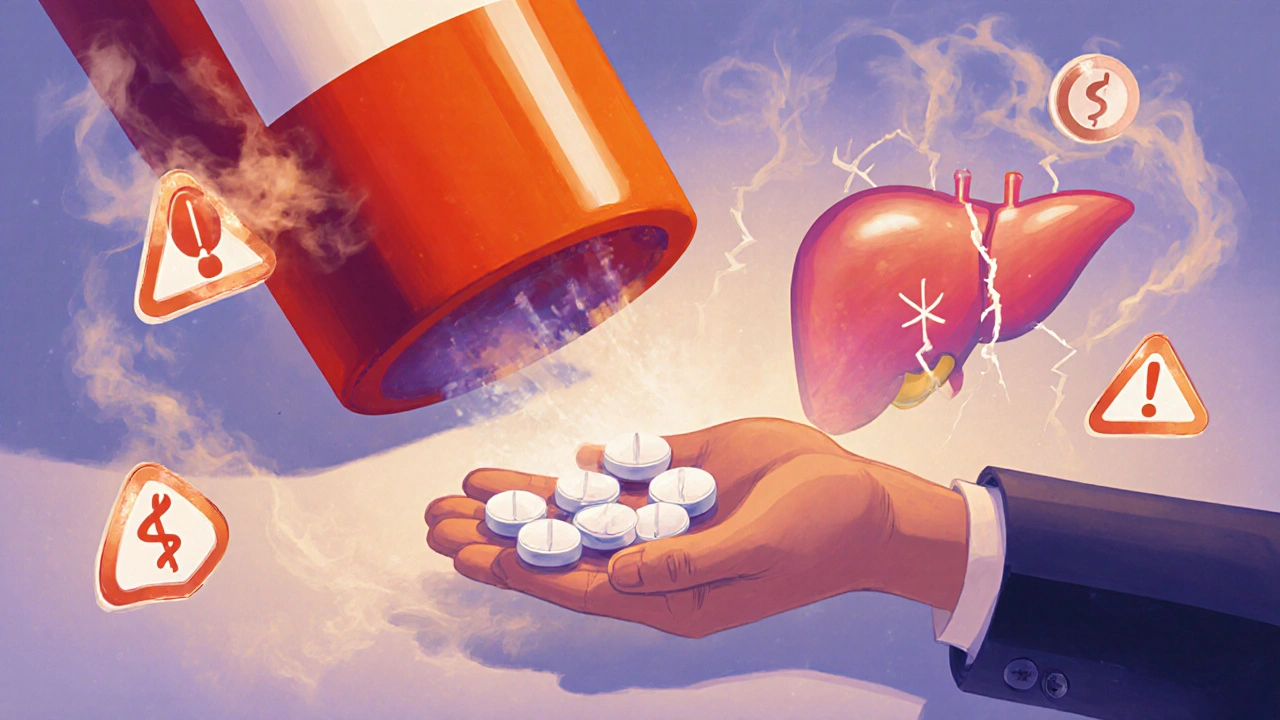
Myth: Over-the-counter meds are completely safe
Many people think if it’s sold on a shelf without a prescription, it’s harmless. That’s not true. Acetaminophen - the active ingredient in Tylenol and hundreds of other pain relievers - causes 56,000 emergency room visits every year in the U.S. alone. Why? Because people take more than they should. The FDA updated the safe daily limit to 3,000 mg in 2011, but many still think 4,000 mg is fine. That’s eight extra-strength tablets. One extra tablet, taken over a few days, can cause severe liver damage. In fact, acetaminophen overdose is responsible for 50% of all acute liver failure cases in the country. It doesn’t happen overnight. It builds up quietly. You might feel fine. Your liver isn’t screaming. But by the time symptoms show up, it’s often too late.
Myth: More pills = better results
If one ibuprofen helps your headache, shouldn’t two or three help more? No. Taking more than the recommended dose - more than 1,200 mg in 24 hours - doesn’t make pain go away faster. It just increases your risk of serious side effects. A 2017 study in JAMA Internal Medicine found that exceeding the dose raises your chance of internal bleeding by 4.5 times. The same goes for naproxen, aspirin, and other NSAIDs. Your body doesn’t store extra medicine for later use. It processes what you take, and the excess just stresses your stomach, kidneys, and heart. Pain relief isn’t a contest. The right dose, taken at the right time, is all you need.
Myth: Stop taking antibiotics when you feel better
This is one of the most dangerous habits. You take antibiotics for a sore throat or sinus infection. After two days, you feel fine. So you toss out the rest. Big mistake. That’s exactly how antibiotic-resistant bacteria are born. The CDC says 30% of antibiotic courses are stopped early. What happens is this: the strongest bacteria die first. The weaker ones survive. They multiply. Soon, the infection comes back - and now it won’t respond to the same drug. These superbugs cause 35,000 deaths annually in the U.S. Antibiotics aren’t like painkillers. They don’t just mask symptoms. They kill or stop bacteria from multiplying. If you don’t finish the full course, you’re helping create the next superbug. Always take every pill, even if you feel great.
Myth: Natural or herbal products are always safe
Just because something comes from a plant doesn’t mean it’s harmless. St. John’s Wort, often taken for mild depression, can make birth control pills 15% to 33% less effective, leading to unplanned pregnancies. Ginkgo biloba, popular for memory, can increase bleeding risk by 50% when mixed with warfarin - a blood thinner. Even garlic supplements can thin your blood. These aren’t rare cases. The National Center for Complementary and Integrative Health found that 65% of supplement users believe herbal products are automatically safe. That’s a myth with real consequences. Herbs are powerful. They interact with prescription drugs. They can overload your liver. Always tell your pharmacist or doctor what supplements you’re taking - even if you think they’re "just natural."

Myth: It’s okay to drink alcohol with meds if you’re careful
"I only have one glass of wine" - that’s what people say. But mixing alcohol with certain medications can be deadly. Opioids like oxycodone or hydrocodone (found in Vicodin or Percocet) already slow your breathing. Alcohol does the same. Together, they can shut down your breathing system completely. A 2020 study in Addiction Biology found this combination increases the risk of respiratory depression by 800%. Even with antidepressants, anxiety meds, or sleep aids, alcohol can make you dizzy, drowsy, or cause sudden blackouts. It doesn’t matter if you’re "responsible." The interaction isn’t about how much you drink. It’s about what’s in the bottle. If your medication label says "avoid alcohol," don’t test it.
Fact: Generic drugs are just as effective as brand names
Many people think generics are cheaper because they’re weaker. That’s false. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must be 80% to 125% bioequivalent - meaning your body absorbs them at nearly the same rate. A 2023 analysis by the American Pharmacists Association confirmed no difference in outcomes between generics and brands for conditions like high blood pressure, diabetes, or depression. The only differences are in color, shape, or inactive fillers - none of which affect how the drug works. Choosing generic saves money without sacrificing safety or effectiveness.
Fact: Always do a "brown bag" review
Bring everything you take - pills, vitamins, herbal teas, creams, even eye drops - to your doctor or pharmacist once a year. This simple step, called a "brown bag review," cuts medication errors by 63%, according to a 2021 study. Most people don’t realize they’re taking two drugs with the same active ingredient. Or they forget they’re on a new blood thinner because it was prescribed by a specialist. Pharmacists see these overlaps instantly. They catch duplicate doses, dangerous interactions, and expired meds. You don’t need to be perfect. Just bring the bag. It’s one of the easiest ways to avoid a hospital visit.
Fact: Use the "Teach-Back" method
After your pharmacist explains your new medication, ask them to watch you explain it back in your own words. This isn’t a test - it’s a tool. A 2020 study of 1,200 patients found that when people could explain their meds correctly, their understanding jumped from 42% to 89%. If you say, "I take this once a day for my blood pressure," and the pharmacist says, "Actually, you take it at night because it can make you dizzy in the morning," you’ve just avoided a fall. Most patients don’t remember everything the first time. Teaching it back helps fix misunderstandings before they become problems.

Fact: Synchronizing refills improves adherence
Trying to keep track of multiple refill dates is exhausting. One med runs out on Tuesday, another on Friday. You miss a dose. You forget. ExactCare Pharmacy tracked 5,000 Medicare patients who switched to synchronized refills - all prescriptions due on the same day each week. Adherence went from 52% to 81%. That’s not magic. It’s convenience. When you know exactly when to pick up your meds, you’re more likely to take them. Ask your pharmacy if they offer this service. It’s free and simple.
Fact: Dosing errors are the #1 medication problem
The Institute for Safe Medication Practices found that 33.7% of all medication errors are dose-related - too much or too little. The second biggest issue? Stopping meds too soon (22.1%). These aren’t accidents. They’re results of misinformation. People think "more is better." They assume "if it’s not hurting, I don’t need it." These myths cost the U.S. healthcare system $42 billion a year in preventable hospital stays. The fix isn’t more technology. It’s better communication. Ask questions. Say "I don’t understand." Write it down. Use a pill organizer. Don’t guess.
Fact: Pharmacists are your medication safety partners
You don’t need to wait until you have a problem to talk to your pharmacist. They’re trained to spot risks before they happen. Whether it’s a new prescription, a supplement you’re trying, or a change in how you feel, your pharmacist is the one person who sees your full medication picture. In 2023, U.S. community pharmacists prevented an estimated 195 million medication-related problems just by talking to patients. That’s more than the population of Canada. They’re not just dispensers. They’re safety monitors. Use them.
What to do next
- Do a brown bag review this month - bring everything you take to your pharmacist.
- Write down the purpose of each medication. Don’t just list names. Write "for blood pressure," "for sleep," "for inflammation."
- Set phone reminders for doses, especially if you take meds multiple times a day.
- Never share your meds. What works for you might hurt someone else.
- Ask your pharmacist: "Is there anything here I shouldn’t mix with alcohol or other supplements?"
Medication safety isn’t about being perfect. It’s about being informed. One question, one conversation, one review can stop a hospital trip. You’re not alone. Your pharmacist is there to help. Use them.


I used to think Tylenol was harmless until my buddy ended up in the ER. Now I count every pill like it's a bullet in a gun. One extra tablet ain't worth it.
OMG YES. 🙌 I used to stop my antibiotics as soon as I felt better... until I got the infection back AND it was resistant. Now I take every single pill like it's my last chance. My pharmacist even gave me a little sticker chart. 🎉💊
Let me tell you something from India - we call this 'dawa ki samajh' - understanding medicine. In my village, people think if it's green and comes from a tree, it's safe. But St. John’s Wort? It can ruin your birth control. And garlic pills? They thin your blood like water. We need more education, not just fear. Talk to your pharmacist, not just Google. 🌿🩺
Wait... so you're saying I can't just take 6 Advil when I have a migraine? And I can't mix wine with my Xanax? And I can't just skip the last 5 pills of my amoxicillin? This is insane. I mean, come on. I'm not a child. Who made all these rules? Who even cares?
I work with elderly patients and this hits hard. One woman was taking three different painkillers - two with acetaminophen - and didn’t know. She didn’t even realize she was double-dosing. We did a brown bag review and found 14 meds she didn’t need. She cried. Not because she was scared, but because she finally felt seen. You don’t need to be perfect. Just be aware.
generic drugs? lol. i took one once and it felt like my body was on vacation. brand name made me feel like a human. also, who even uses a brown bag anymore? i just throw everything in my gym bag and hope for the best
This article is just fearmongering dressed up as 'education.' People are dying from 'medication errors'? Please. It's the pharma companies and the FDA that are the real problem. You're being manipulated into trusting the system that overprescribes and overcharges. Take responsibility for your own body. Not some pharmacist's checklist.
I did a brown bag review last week and found three expired pills and two I forgot I was even taking. 🤯 My pharmacist laughed and said, 'This is why I have a job.' So glad I did it. No drama, just relief.
Bro, the teach-back method? That’s gold. I’m a med student in Mumbai and we train our patients to repeat back the instructions. One guy said he was taking his BP med ‘after breakfast’ - turned out he meant after his chai, which was at 11 PM. We fixed it. No more dizziness. Simple. Human. Effective. 🙌