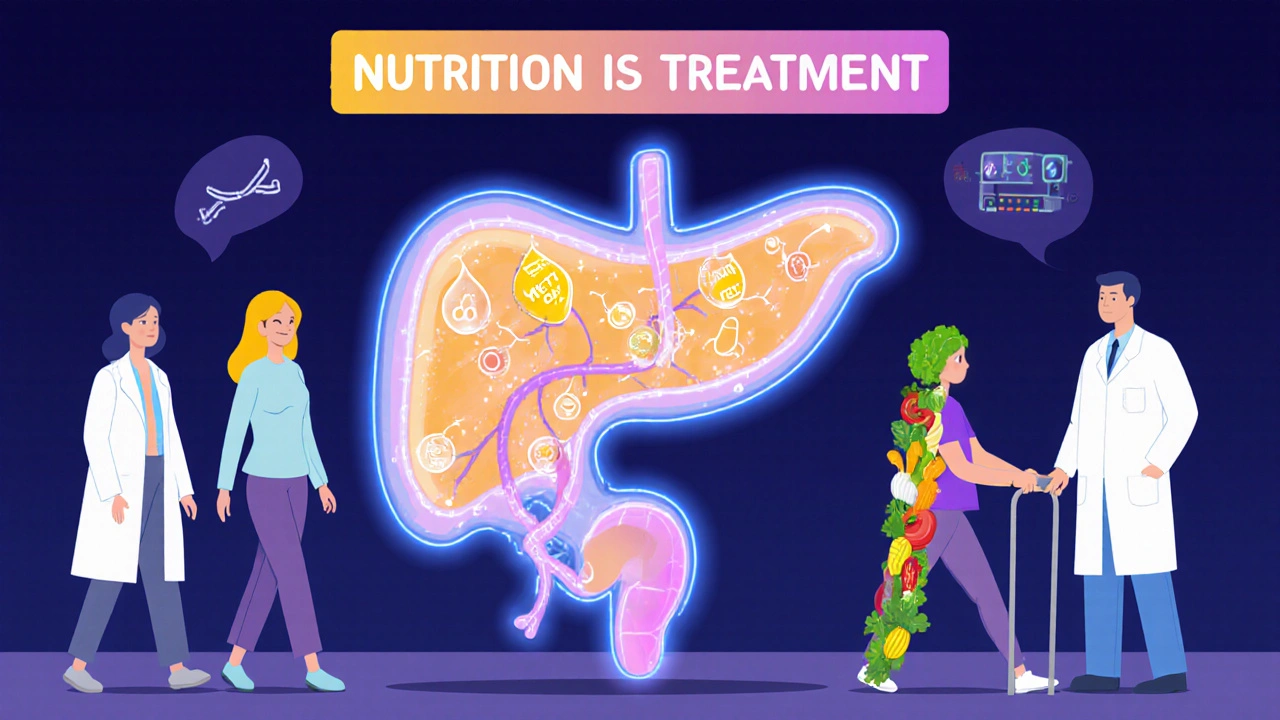
When your pancreas inflames, it doesn’t just hurt-it disrupts everything. Digestion slows, blood sugar swings, and food that once felt safe can trigger agony. Pancreatitis isn’t one condition. It’s two very different diseases with the same name: acute and chronic. One comes on fast, often after a night of heavy drinking or a gallstone attack. The other creeps in silently, eating away at your pancreas over years. And whether you’re dealing with the sudden flare or the long-term damage, nutrition isn’t just helpful-it’s the foundation of recovery.
Acute Pancreatitis: The Sudden Fire
Acute pancreatitis hits like a storm. One moment you’re fine. The next, you’re doubled over with sharp pain in your upper belly, radiating to your back. Nausea, vomiting, fever-these aren’t just bad stomach bugs. They’re signs your pancreas is digesting itself. That’s what happens when digestive enzymes, meant to break down food in the small intestine, get activated too early-inside the pancreas. The organ starts tearing itself apart.
Most cases (about 80%) are caused by gallstones or alcohol. The rest? Sometimes it’s medications, high triglycerides, or even unknown reasons. Doctors diagnose it with three things: your pain pattern, blood tests showing lipase or amylase levels three times higher than normal, and a CT or ultrasound showing swelling or fluid around the pancreas.
Here’s the good news: most people bounce back in a week. But severity matters. Mild cases? You’re likely out of the hospital in a few days. Severe cases? That’s when things turn dangerous. Organ failure-lungs, kidneys, heart-can kick in. About 15% of severe cases end in death. The key? Early, aggressive hydration. Studies show getting fluids into you within the first 24 hours cuts the risk of tissue death and infection by nearly a third.
Food? You won’t eat right away. Your body needs to rest. But don’t wait too long. Starting enteral nutrition (tube feeding directly into the small intestine) within 24 to 48 hours reduces infections and speeds healing. Going without food for days? That actually increases complications.
Chronic Pancreatitis: The Slow Burn
Chronic pancreatitis is a different beast. It doesn’t vanish after a week. It lingers. And it doesn’t just hurt-it breaks you down. Your pancreas turns scarred, calcified, and useless. Enzymes? They’re gone. Digestion? Broken. Blood sugar? Unstable. And the pain? It becomes a constant shadow.
Alcohol is the biggest cause-up to 90% of cases show clear signs of long-term use. But genetics play a role too. Mutations in genes like PRSS1 or SPINK1 can make you vulnerable even if you never touch alcohol. Smoking? It doesn’t just cause cancer. It makes chronic pancreatitis progress twice as fast. Quitting is the single most effective thing you can do to slow it down.
Doctors track progression in stages. Early on, you have flare-ups but still digest food okay. Then comes the middle phase: you start losing weight, your stools become greasy and foul-smelling (steatorrhea), and you’re constantly bloated. By the late stage, the pain may even fade-but now you’re diabetic and can’t digest fats, proteins, or vitamins at all.
That’s where nutrition becomes life-or-death. Without enzymes, your body can’t absorb nutrients. You lose muscle. You get weak. Your bones thin from vitamin D deficiency. Your nerves suffer from B12 loss. Studies show 85% of chronic pancreatitis patients are low in vitamin D. Four in ten lack B12. One in four is deficient in vitamin A.
Nutrition for Acute Recovery: Rebuilding from Ground Zero
After the acute flare settles, you’re not done. Your pancreas is still healing. You can’t jump back into burgers and fries. The goal? Gentle, consistent fuel that doesn’t overload your system.
Start with clear liquids-water, broth, electrolyte drinks. Then move to bland, low-fat foods: rice, toast, applesauce, boiled chicken. Don’t rush. Wait until your pain is gone, your nausea is under control, and your bowel movements are normal before adding more.
Calorie and protein needs? Around 30 to 35 calories per kilogram of body weight each day. That’s about 1.5 grams of protein per kilogram. For a 70kg person, that’s 2,100 to 2,450 calories and 105 grams of protein daily. Spread it out. Eat small meals every 2 to 3 hours. Your pancreas can’t handle big loads.
Fat? Keep it low-under 30 grams a day during recovery. Avoid fried foods, butter, cream, fatty meats. You’re not cutting fat forever, but your pancreas needs time to recover before handling it again.
And don’t skip vitamins. Even if you’re eating well, your body’s absorbing less. A daily multivitamin with zinc, selenium, and antioxidants can help reduce inflammation and support healing.
Nutrition for Chronic Management: Surviving with a Broken Pancreas
If you have chronic pancreatitis, you’re managing a lifelong condition. Your pancreas won’t heal. But you can still live well-if you get nutrition right.
First: pancreatic enzyme replacement therapy (PERT). This isn’t optional. It’s mandatory. You need to take enzyme pills with every meal and snack. Dosing? 40,000 to 90,000 lipase units per main meal, 25,000 per snack. That’s not a suggestion-it’s medical protocol. Studies show proper dosing cuts fatty stools by 40 to 60%.
But here’s the catch: enzymes don’t work if you take them wrong. Take them right before you start eating. Don’t crush them. Don’t mix them with hot food. Swallow them whole with water. If you’re still having greasy, floating stools, your dose is too low. Talk to your doctor. Get a fecal fat test to check.
Second: fat intake. You need fat-it’s essential. But you need the right kind. Medium-chain triglycerides (MCTs) don’t need pancreatic enzymes to be absorbed. They go straight to your liver. Use MCT oil in smoothies, drizzle it on soups, or add it to oatmeal. Avoid long-chain fats like butter, cheese, and fried chicken.
Third: eat small, often. Six to eight mini-meals a day. Why? Your pancreas can’t handle big surges. Smaller meals mean less enzyme demand, less pain, better absorption.
Fourth: watch your blood sugar. Over half of chronic pancreatitis patients develop diabetes within 12 years. Use complex carbs-oats, quinoa, sweet potatoes-not white bread or sugar. Monitor glucose. The FDA approved the Dexcom G7 CGM in 2024 specifically for pancreatogenic diabetes. It’s a game-changer for catching swings before they crash you.
Fifth: supplement aggressively. Vitamin D, B12, A, E, K, zinc, magnesium-test them every 6 to 12 months. Deficiencies don’t show up until you’re already damaged. Don’t wait for weakness or numbness to start taking them.
What Not to Do
Don’t ignore alcohol. Even one drink can trigger a flare in chronic pancreatitis. It’s not about moderation-it’s about elimination.
Don’t rely on over-the-counter enzymes. Most aren’t strong enough. You need prescription-grade PERT like Creon or Zenpep.
Don’t avoid food out of fear. Starving yourself doesn’t help your pancreas. It starves your body. You’ll lose muscle, get weaker, and heal slower.
Don’t assume your doctor knows how to manage this. Only 35% of primary care doctors feel confident treating chronic pancreatitis. Find a specialist. Go to a pancreatic center. Johns Hopkins, Mayo Clinic, University of Pittsburgh-they have dedicated teams. Nutritionists, pain specialists, endocrinologists-all working together.
Real Stories, Real Results
Sarah, 52, spent seven years misdiagnosed. She lost 40 pounds. Her stools were uncontrollable. Then she found the Johns Hopkins Pancreatitis Center. They switched her to MCT oil and adjusted her enzyme dose. Her fatty stools dropped from 4-5 times a day to 1-2 weekly. She gained 15 pounds back.
Mark, 47, took 40,000 LU of enzymes daily but still lost 35 pounds. He ended up in the hospital on a feeding tube. His solution? A higher dose-70,000 LU per meal-and switching to a liquid meal supplement with MCTs. He’s off the tube now. Still managing, but alive.
They didn’t get better because they took pills. They got better because they got the right nutrition plan-and stuck to it.
The Bigger Picture
Pancreatitis isn’t just about pain. It’s about survival. Acute pancreatitis can kill in days. Chronic pancreatitis kills slowly-through malnutrition, diabetes, and cancer. The risk of pancreatic cancer? 15 to 20 times higher than normal. That’s why annual MRIs are now recommended for chronic patients.
But here’s the hope: you can change the trajectory. Quit smoking. Take your enzymes. Eat the right fats. Test your vitamins. Work with a team. Nutrition isn’t a side note-it’s your treatment plan. And when you treat it like that, you don’t just survive. You live.


Yo, this post is a godsend. I’ve been through acute pancreatitis twice, and nobody ever told me about enteral nutrition being a game-changer. I thought starving myself was the plan-turns out, it was making things worse. Started tube feeding after day 2, and my recovery time halved. Also, MCT oil? Life hack. I drizzle it on everything now-oatmeal, scrambled eggs, even my coffee (yes, really). My doc thought I was crazy. Now he’s prescribing it to others. Nutrition isn’t just support-it’s the damn treatment.
And for anyone thinking ‘I’ll just cut fat forever’-nope. You need fats. Just the right kind. MCTs are the unsung heroes here. Don’t let fear starve you.
Also, if you’re still using OTC enzymes, stop. You’re wasting money and time. Creon isn’t expensive compared to a hospital stay. Trust me.
PS: Quit smoking. Even one cigarette a day speeds up the decay. I did it. Still alive. Still cooking.
PPS: Vitamin D levels? Get them checked. I was at 12 ng/mL. Now I’m at 58. I can feel the difference in my bones. Seriously.
PPPS: Johns Hopkins? They saved me. Don’t wait until you’re on a feeding tube. Go early.
PPPPS: If you’re reading this and scared? You’re not alone. We’re all just trying to eat without crying.
Wow. So… eating less fat is now medical advice? Groundbreaking.
This is just a glorified ad for Creon and MCT oil. Nobody talks about how 80% of these ‘success stories’ are cherry-picked. You think people with chronic pancreatitis just need to ‘take enzymes’? Try living with 12-hour pain cycles while your pancreas turns to concrete. And don’t get me started on the vitamin nonsense-supplements don’t fix organ failure. This post reads like a pharma pamphlet written by someone who’s never held a patient’s hand during a flare.
Also, ‘don’t rely on OTC enzymes’? Funny. I’ve been taking Now Foods pancreatic enzymes for 5 years. I’m not dead. Maybe your ‘protocol’ is just corporate dogma dressed up as science.
I appreciate the depth here, and I know this stuff saves lives. But I also know how overwhelming this info can be for someone newly diagnosed. The fear of messing up a meal, the guilt when you can’t eat normally, the shame when you lose weight… it’s not just physical. I’ve seen people quit PERT because they felt like failures when they still had greasy stools. It’s not about perfection-it’s about consistency. One pill, one meal, one day at a time.
And yes, MCT oil sounds weird, but it’s not magic. It’s just chemistry working for you. Same with the enzymes. They’re not a cure, but they’re the best tool we’ve got. If you’re struggling, find a dietitian who specializes in pancreatic care. They’re rare, but they exist. And they’ll help you adjust without making you feel broken.
You’re not failing. You’re adapting. And that’s enough.
Just wanted to say THANK YOU for this. My dad had chronic pancreatitis for 11 years. We thought he was just ‘always tired’ until we found out he was vitamin deficient in 5 things. He started MCT oil in his smoothies and switched to Creon. He went from 118 lbs to 152. He’s still alive. He’s still hiking. He still makes terrible pancakes (but they’re low-fat, so he says it’s ‘healthy’ 😅).
This post gave me hope. I’m sharing it with everyone I know who’s dealing with this. You didn’t just write an article-you wrote a lifeline.
Also, Dexcom G7? I just ordered one for him. He’s gonna hate wearing it, but if it stops another ER trip? Worth it.
❤️
While I appreciate the clinical detail, I must point out that the overwhelming reliance on American medical protocols-particularly the obsession with MCT oil and prescription enzymes-is both culturally myopic and economically exploitative. In the UK, we manage pancreatitis with dietary moderation, NHS-supervised enzyme therapy, and a far more restrained approach to supplementation. The notion that one must consume 90,000 lipase units per meal is not only excessive, it is a symptom of American healthcare’s profit-driven over-interventionism.
Furthermore, the glorification of Johns Hopkins as a panacea ignores the fact that many European centres achieve comparable outcomes with less invasive protocols. We do not need to be ‘saved’ by American specialists-we need to be freed from their marketing.
lol so if i dont take 70k lu of enzymes i’m just gonna die? also i’m supposed to eat 8 meals a day? what am i, a goldfish? and why is everyone acting like this is new info? i’ve had this since 2015 and no one ever told me about mct oil until now? lol.
also i quit smoking and still got it so… yeah. thanks for the guilt trip.
and who the hell is this sarah and mark? are they even real? or just marketing ploys? 🤡
Stop saying ‘don’t rely on OTC enzymes.’ That’s not helpful. It’s condescending. Many of us can’t afford Creon. And yes, some OTC brands work fine for mild cases. You’re not helping by shaming people who can’t access expensive meds. This post reads like a pharmaceutical sales pitch dressed as empathy.
Let’s be real-this whole post is a miracle cure fantasy. Acute pancreatitis? Yeah, hydration helps. But 15% mortality? That’s not ‘early hydration’ saving you-that’s luck. And chronic? You think enzymes are a fix? They’re a band-aid on a ruptured artery. You’re not ‘living well’-you’re surviving on a treadmill of pills, oils, and blood tests. And the cancer risk? 15-20x higher? That’s not ‘hope’-that’s a death sentence with a side of MCT oil.
Stop romanticizing this. This isn’t a wellness blog. It’s a chronicle of slow decay. And the people who say ‘I’m living well’? They’re either lying or they haven’t hit stage three yet.
Also, ‘don’t ignore alcohol’? Tell that to the guy who lost his job, his family, and his dignity trying to quit. This post doesn’t address trauma. It just gives a checklist. That’s not care. That’s capitalism.
Look-I get it. You’re trying to help. And honestly? You did a great job laying this out. But let’s talk about the elephant in the room: this isn’t just about nutrition. It’s about access. Not everyone can afford Creon. Not everyone has a dietitian on speed dial. Not everyone can afford MCT oil or a Dexcom G7. And for people living paycheck to paycheck? The ‘right’ way to eat is a luxury.
I’ve seen people skip meals because they couldn’t afford the enzymes. I’ve seen people use expired supplements because they had no choice. This isn’t failure. It’s systemic.
So while I’m grateful for the science here, I’m also angry that the ‘solution’ is so expensive. The real win? Making enzymes affordable. Making specialists accessible. Making nutrition care part of public health-not a privilege.
Let’s not just tell people what to do. Let’s make sure they can do it.
And if you’re reading this and you’re struggling? You’re not broken. The system is. Keep going. Even if it’s just one meal. One pill. One day.
And if you can? Fight for change. Because no one should have to choose between food and medicine.
And to the person who said ‘I can’t afford Creon’-I hear you. I was there. I applied for patient assistance programs. Got Creon free for 18 months. Talk to your pharmacist. Ask for samples. Call the manufacturer. They help more than you think. I didn’t know that until I begged. You’re not weak for asking. You’re smart.
Also-MCT oil isn’t expensive. A bottle lasts months. It’s cheaper than a single ER visit. And if you’re still using OTC? Fine. Just don’t lie to yourself. If your stools are still floating? You need more. Ask your doc to titrate. No shame. Just action.
We’re all just trying to eat without crying. Let’s not make it harder by pretending money doesn’t matter. It does. But it doesn’t have to win.