Goldenseal Medication Interaction Checker
Check Your Medication Risk
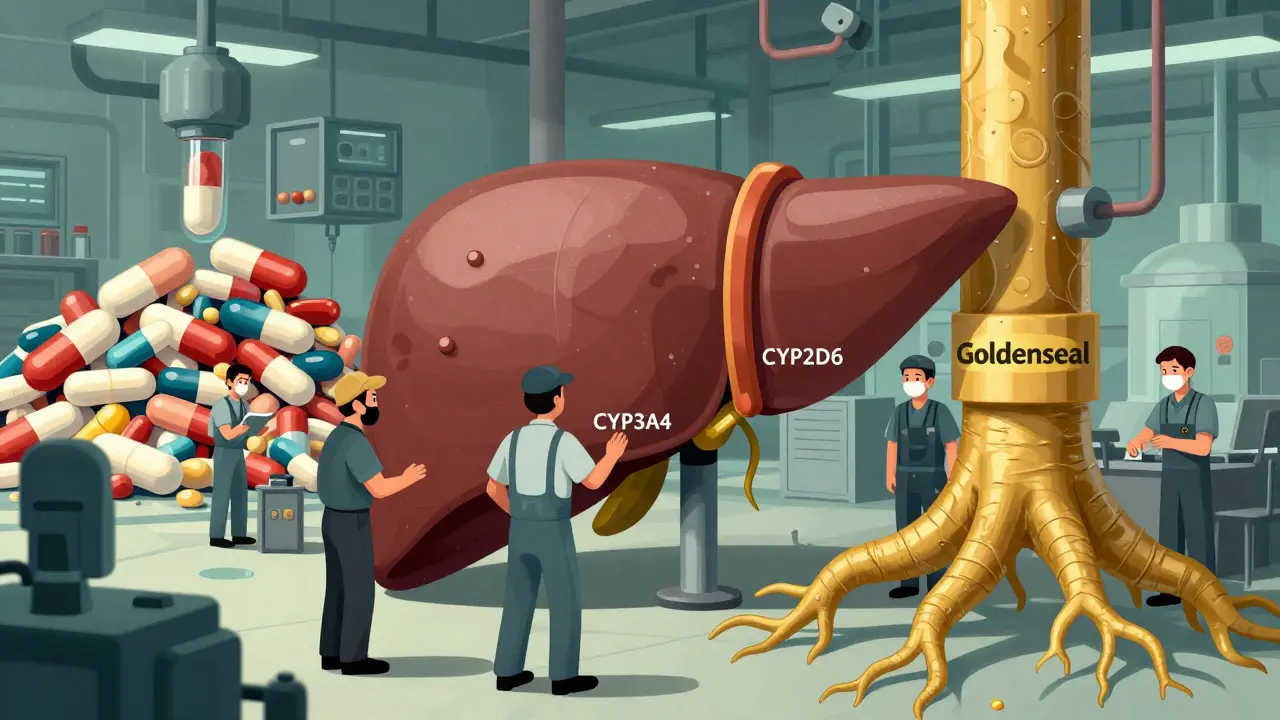
Goldenseal inhibits key liver enzymes (CYP3A4, CYP2D6, etc.) that process 75% of prescription drugs. This tool checks if your medications could interact dangerously with goldenseal.
Most people take goldenseal because they believe it boosts immunity or clears up a cold. But what they don’t realize is that this popular herb can quietly mess with their medications - sometimes with dangerous results. If you’re on blood pressure pills, diabetes drugs, antidepressants, or even statins, goldenseal might be hiding a silent risk in your supplement cabinet.
What Goldenseal Actually Does in Your Body
Goldenseal comes from the root of a plant called Hydrastis canadensis, native to the eastern U.S. For over a century, it’s been used in traditional medicine for infections, digestive issues, and inflammation. Today, it’s sold in capsules, teas, and tinctures as a “natural immune booster.” But the science tells a different story.
The real actors behind its effects are two alkaloids: berberine and hydrastine. These compounds don’t just fight germs - they interfere with how your liver breaks down drugs. Specifically, they block key enzymes called cytochrome P450 (CYP), which handle about 75% of all prescription medications. Think of these enzymes as the liver’s recycling crew. When goldenseal shuts them down, your meds don’t get processed properly.
It doesn’t just affect one enzyme. Goldenseal hits five major ones: CYP3A4 (which processes half of all drugs), CYP2D6 (responsible for 30% of prescriptions), CYP2C9, CYP1A2, and CYP2E1. That’s unusual. Most herbs only mess with one or two. Goldenseal? It’s a multi-target blocker.
Why This Matters for Your Medications
If your liver can’t break down your medication, it builds up in your blood. That’s not good. It can turn a safe dose into an overdose - without you even knowing.
Take statins like simvastatin or atorvastatin. These lower cholesterol, but they’re metabolized by CYP3A4. If you take goldenseal, your statin levels can spike, raising your risk of muscle damage, kidney failure, or even rhabdomyolysis - a life-threatening condition.
What about blood pressure meds? Drugs like lisinopril and metoprolol are broken down by CYP2D6. A 2018 clinical trial showed goldenseal can raise metoprolol levels by up to 60%. One Reddit user reported fainting and a blood pressure drop to 85/50 after combining goldenseal with lisinopril - and ended up in the ER.
Then there’s warfarin, the blood thinner. Goldenseal can push INR levels up by 1.5 to 2.0 points, increasing bleeding risk. The Merck Manual warns about this specifically. Even small changes in INR can lead to internal bleeding.
And don’t forget diabetes drugs. Metformin is transported by P-glycoprotein - a system goldenseal also blocks. But here’s the twist: in one documented case, a diabetic patient’s metformin levels dropped by 25% after taking goldenseal. His HbA1c jumped from 6.8% to 8.2% in four weeks. Why? Because the herb’s effects are unpredictable. Berberine levels in supplements vary wildly - from 0.5% to 8% - so you can’t guess how it’ll affect you.
How Goldenseal Compares to Other Herbs
Not all herbs are created equal when it comes to interactions. St. John’s Wort, for example, is notorious - but it works differently. It induces enzymes, meaning it speeds up drug breakdown and makes meds less effective. Goldenseal does the opposite: it inhibits them, causing dangerous buildup.
Compared to milk thistle (which mainly affects CYP2C9) or grapefruit juice (which mainly blocks CYP3A4), goldenseal is broader. A 2020 review ranked it as the third-highest risk herbal supplement for drug interactions - behind only St. John’s Wort and grapefruit juice. But unlike grapefruit juice, which you can avoid by skipping breakfast, goldenseal is often taken daily as a “wellness” habit. That’s the problem.
And unlike St. John’s Wort, which has clear warning labels in many countries, goldenseal is sold with little to no caution. Most bottles say “support immune health” - nothing about liver enzymes, drug interactions, or bleeding risks.

Who’s at Risk?
You’re at higher risk if you:
- Take any medication metabolized by CYP3A4, CYP2D6, CYP2C9, CYP1A2, or CYP2E1
- Have liver disease or reduced liver function
- Take multiple medications at once
- Are over 45 - the age group most likely to use goldenseal regularly
- Use supplements from brands that don’t verify their ingredients
A 2022 USP study found only 38% of goldenseal supplements contained berberine within 20% of what was on the label. That means you could be getting half the dose - or five times more - than expected. No one knows what they’re really taking.
What Doctors Say
The American Academy of Family Physicians doesn’t mince words: they recommend against using goldenseal with most medications. Dr. Edzard Ernst, a leading expert in complementary medicine, called it “one of the most dangerous herbal supplements” because its interaction profile is worse than many prescription drugs.
The FDA has issued warning letters to 12 supplement makers for claiming goldenseal treats infections - because there’s no solid proof it does. Yet it’s still sold everywhere: pharmacies, health food stores, Amazon. The U.S. market sold $18.7 million worth of goldenseal in 2022. That’s a lot of people taking something with no proven benefit - and real, documented risks.
Even integrative medicine experts like Dr. Tieraona Low Dog admit the risks outweigh the benefits. “The lack of standardization and significant interaction potential make clinical use problematic,” she wrote in 2019.

What Should You Do?
Here’s the simple rule: Don’t take goldenseal if you’re on any prescription medication. Period.
If you’re already taking it:
- Stop immediately.
- Wait at least two weeks before restarting any medication - goldenseal’s effects linger for 7 to 14 days.
- Talk to your pharmacist or doctor. Bring your supplement bottle. Ask: “Which of my meds are metabolized by CYP3A4 or CYP2D6?”
Use the American Society of Health-System Pharmacists’ free online CYP interaction checker. It lists 147 medications with known or possible interactions with goldenseal - updated quarterly. You don’t need to guess. The data is there.
For acute colds or sinus infections, stick to proven options: saline rinses, rest, hydration. Goldenseal isn’t necessary. And if you’re considering it for long-term immune support - there’s no good evidence it works. The FDA says so. The science says so.
The Bigger Picture
The supplement industry is booming. But regulation is weak. Companies don’t have to prove safety before selling. They just have to say “this isn’t a drug.” That loophole lets goldenseal stay on shelves - even though it can cause hospitalizations.
The NIH is running a $2.3 million clinical trial (NCT05578231) to study goldenseal’s interactions with 10 common drugs. Results won’t be out until late 2025. But we already know enough to act. You don’t need another study to avoid a dangerous interaction.
There’s a reason the European Medicines Agency banned goldenseal from medicinal products. They didn’t wait for more data. They acted on what was already clear: the risks are real, the benefits are unproven, and the variability is too high to manage safely.
If you’re healthy and not on any meds, a short 3-5 day course might be low risk - but even then, you’re gambling with an unregulated product. Most positive reviews on Amazon mention users only took it when not on prescriptions. That’s telling.
There’s no such thing as a “natural” supplement that’s harmless. Nature doesn’t care about your prescription. It only cares about chemistry. And goldenseal’s chemistry is a minefield.


I used to take goldenseal every winter thinking it kept me from getting sick. Turned out I was just lucky. After I started on metoprolol and kept taking it, I nearly passed out on the subway. My pharmacist caught it when I brought in my bottle. Never again.
It is an absolute disgrace that the United States permits the sale of unregulated botanicals with such demonstrable pharmacological danger. The FDA’s inaction constitutes a dereliction of duty. Compare this to the European Medicines Agency’s decisive ban - a reflection of scientific rigor versus American regulatory negligence.
Anyone else notice how goldenseal is always marketed as "natural immunity" but never says "this might kill your statin"? I checked my bottle - no warning. Just a picture of a pretty root. The supplement industry is built on ignorance. I’ve started asking my doctor about every supplement now - even the ones that seem harmless.
Stop taking it if you're on meds.
Wait two weeks.
Talk to your pharmacist.
Use the CYP checker.
That's it.
People still buy this stuff? Honestly, it's not just ignorance - it's willful denial. You read a blog post about "ancient healing wisdom," see a testimonial from someone who "felt better," and suddenly you think you're above pharmacology. The fact that this herb is sold in the same aisle as protein powder is a national embarrassment. And don't even get me started on the brands that don't even test their berberine content. You're not taking a supplement - you're playing Russian roulette with your liver enzymes.
Thanks for laying this out so clearly. I’ve been on blood pressure meds for years and never thought twice about the herbal stuff I’d take. This post made me pause and actually check my bottle. I’m stopping it today. Better safe than sorry.
It's funny how we trust plants more than science. We call them "natural" like that makes them safe. But nature gave us poison ivy and hemlock too. Chemistry doesn't care if it's from a root or a lab. Goldenseal isn't evil - it's just powerful and uncontrolled. And that's the real danger.
Did you know the FDA doesn't regulate supplements because Big Pharma owns them? Goldenseal is dangerous because they want you to keep taking pills. The real cure is in nature - but they profit from your sickness. This whole thing is a cover-up. The NIH study? A distraction. They don't want you to know that a $5 root can outsmart their billion-dollar drugs.
Thank you for this thoughtful and scientifically grounded post. 🙏 I am from India, where herbal remedies are deeply embedded in culture, but I now understand that tradition must be balanced with pharmacological evidence. I will share this with my family who use goldenseal regularly. Safety first, always.
Per the CYP450 enzyme kinetics literature, berberine acts as a competitive inhibitor of CYP3A4 with a Ki of approximately 2.1 μM, and as a non-competitive inhibitor of CYP2D6 with a Ki of 4.8 μM - both well within clinically relevant plasma concentrations achieved with standard goldenseal dosing (1–3 g/day). Furthermore, P-glycoprotein inhibition by hydrastine contributes to altered pharmacokinetics of metformin, which explains the paradoxical reduction in bioavailability observed in the case report you cited. The variability in berberine content (0.5–8%) correlates with interindividual differences in CYP inhibition, making personalized risk stratification nearly impossible without pharmacogenetic testing. Thus, the recommendation to avoid goldenseal entirely in polypharmacy patients is not merely prudent - it is pharmacokinetically obligatory.