SNRI Side Effect Risk Calculator
Select your SNRI medication and dosage to see potential side effects and risk levels.
Side Effect Risk Profile
| Medication Feature | Venlafaxine | Duloxetine |
|---|---|---|
| Best For | Generalized anxiety, depression | Chronic pain (neuropathy, fibromyalgia) |
| Side Effect Profile | More likely to cause BP spikes at higher doses | Higher initial nausea, but gentler on heart |
| Withdrawal Risk | High (54% report severe symptoms) | Moderate (less than venlafaxine) |
| Weight Changes | Often weight loss initially, possible gain later | Weight loss common in first few months |
When you’re struggling with depression and chronic pain at the same time, finding a medication that helps both can feel like a breakthrough. That’s where SNRI medications come in. Unlike older antidepressants that only target serotonin, SNRIs - serotonin-norepinephrine reuptake inhibitors - work on two key brain chemicals at once. This dual action makes them uniquely useful for people who don’t just feel low emotionally, but also carry the heavy weight of constant physical pain. Venlafaxine, duloxetine, and others in this class are now among the most commonly prescribed antidepressants worldwide, not just for mood, but for nerve pain, fibromyalgia, and anxiety disorders too.
How SNRIs Actually Work in Your Brain
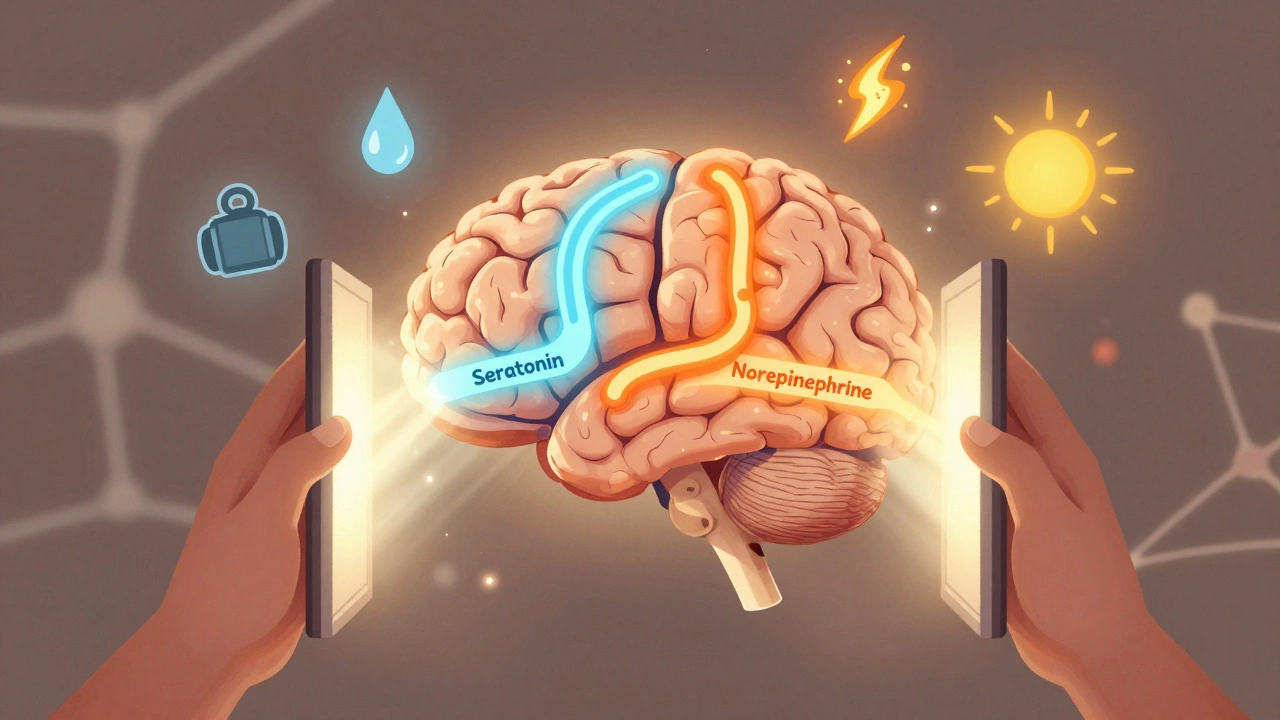
SNRIs don’t create new neurotransmitters. Instead, they stop your brain from reabsorbing serotonin and norepinephrine too quickly. Think of it like holding open a door so these mood-boosting chemicals can stay longer in the space between nerve cells. Serotonin helps with emotional balance, sleep, and appetite. Norepinephrine is linked to energy, focus, and how your body responds to stress. When both are in short supply, you might feel tired, numb, or overwhelmed - even if nothing ‘bad’ has happened.
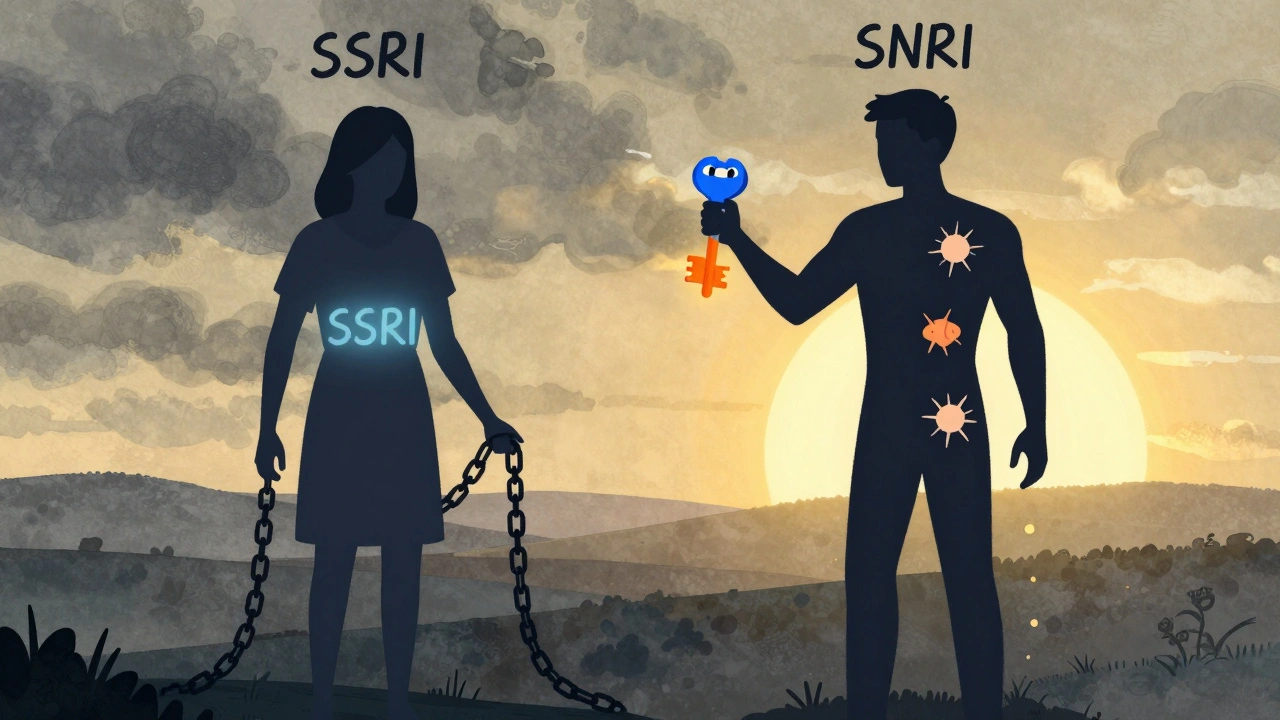
The real advantage of SNRIs over SSRIs (which only affect serotonin) is that they also lift norepinephrine. That’s why people often report feeling more alert and less foggy on SNRIs. It’s not just about feeling less sad - it’s about feeling like yourself again. This dual effect is also why SNRIs are approved for diabetic neuropathy, fibromyalgia, and chronic back pain. SSRIs rarely help with those. A 2023 review from Elsevier Health found that duloxetine and venlafaxine have strong evidence for reducing pain signals in the nervous system, not just improving mood.
Venlafaxine: The Original SNRI
Venlafaxine (sold as Effexor XR) was the first SNRI approved in 1993. It’s still one of the most prescribed antidepressants in the U.S., with over 22 million prescriptions annually. What sets venlafaxine apart is how its effect changes with dosage. At low doses (under 75mg), it acts mostly like an SSRI - targeting serotonin. But as the dose climbs above 150mg, it starts strongly blocking norepinephrine reuptake too. That’s why doctors often start low and go slow.
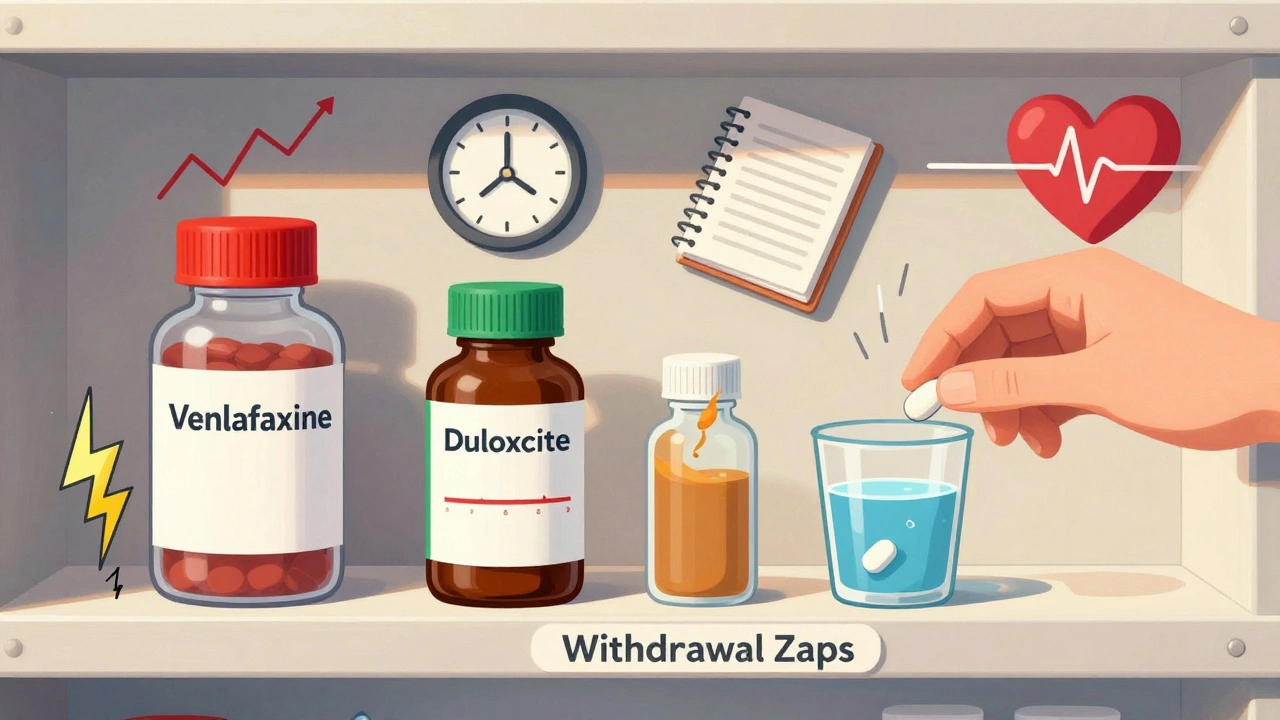
Many users report venlafaxine gives them a noticeable energy boost compared to SSRIs. But there’s a catch. Higher doses come with a higher risk of high blood pressure. Around 12-15% of people taking more than 150mg daily develop hypertension, according to the Cleveland Clinic. That’s why regular blood pressure checks are recommended if you’re on a higher dose. Also, venlafaxine has a reputation for tough withdrawal symptoms. If you miss a dose or stop suddenly, you might get brain zaps, dizziness, nausea, or even flu-like symptoms. About 54% of users on Reddit and Drugs.com report this ‘venlafaxine cliff’ - a sudden drop in mood and physical discomfort that can feel terrifying.
Duloxetine: The Pain-Focused SNRI
Duloxetine (Cymbalta, Drizalma Sprinkle) is the SNRI most often prescribed for pain. It’s FDA-approved for depression, generalized anxiety, diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain. That’s more conditions than any other SNRI. People who’ve tried multiple antidepressants and still have body aches often find duloxetine helps where others failed.
But it comes with a strong start. Around 25-30% of users get nausea in the first week or two. It’s usually mild and fades after 2-4 weeks. Some people lose 5-7 pounds in the first few months, then gain it back later. Dry mouth and sweating are common too - about 30% and 20% of users respectively. Sexual side effects are just as frequent as with other antidepressants: 65% of users report lower libido or trouble reaching orgasm.
What makes duloxetine different is its balanced action. It’s about 10 times more selective for serotonin than norepinephrine, making it less likely to spike blood pressure than venlafaxine. That’s why it’s often preferred for older adults or people with heart concerns. Still, it’s not risk-free. Like all SNRIs, it increases bleeding risk by reducing serotonin in platelets. That’s why you should tell your doctor if you’re on blood thinners or planning surgery.
Other SNRIs: What You Should Know
There are two more SNRIs you might hear about: desvenlafaxine and levomilnacipran. Desvenlafaxine (Pristiq) is basically the active metabolite of venlafaxine. It’s marketed as having fewer side effects, but studies show it’s just as likely to cause nausea, dizziness, and sexual problems. The big difference? It doesn’t need dose adjustments based on liver function, which can be helpful for older patients.
Levomilnacipran (Fetzima) and milnacipran (Savella) are the most norepinephrine-focused SNRIs. Levomilnacipran is about twice as strong at blocking norepinephrine reuptake as serotonin. That makes it potentially better for fatigue and lack of motivation - but also more likely to raise blood pressure and heart rate. Milnacipran is approved only for fibromyalgia in the U.S., not depression. It’s used more in Europe and Japan. Both are less commonly prescribed, partly because they’re more expensive and not as well-known.
Common Side Effects - And How to Handle Them
Almost everyone on SNRIs experiences at least one side effect early on. Here’s what’s most common:
- Nausea: Happens in up to 30% of users, especially with duloxetine. Take with food. It usually fades in 2-4 weeks.
- Sexual problems: Affects 20-40% of users. Lower libido, delayed orgasm, or erectile dysfunction. This is the #1 reason people stop SNRIs. Talk to your doctor - sometimes lowering the dose helps.
- Dizziness and lightheadedness: Especially when standing up fast. Move slowly. Stay hydrated.
- Sweating: More common with duloxetine. Wear breathable clothes. Use clinical-strength antiperspirant.
- Constipation: Affects about 15%. Increase fiber and water. Don’t ignore it - it can get worse.
- Increased blood pressure: Mainly with venlafaxine over 150mg/day. Get your BP checked every few weeks if you’re on a high dose.
Less common but serious: serotonin syndrome. This happens when SNRIs are mixed with other serotonergic drugs - like tramadol, certain migraine meds, or St. John’s Wort. Symptoms include confusion, rapid heart rate, high fever, muscle rigidity, and seizures. It’s rare - about 1 in 1,000 patient-years - but life-threatening. Always tell your doctor everything you’re taking.
Discontinuation Syndrome - Don’t Stop Cold Turkey
Stopping SNRIs suddenly is one of the biggest mistakes people make. About 40-50% of users experience withdrawal symptoms if they quit without tapering. These aren’t ‘psychological’ - they’re physical. Brain zaps (electric shock feelings), headaches, nausea, insomnia, and extreme anxiety can hit within days. Some people feel like they’re having a nervous breakdown.
Doctors recommend tapering over 2-4 weeks. For venlafaxine, that might mean going from 150mg to 75mg, then 37.5mg, then stopping. For duloxetine, you might drop from 60mg to 30mg before stopping. Even then, some people still feel off for weeks. If you’re thinking of quitting, talk to your prescriber first. There’s no shame in needing time to come off safely.
SNRIs vs. Other Antidepressants
Compared to SSRIs like sertraline or fluoxetine, SNRIs are more likely to help with energy, focus, and physical pain. But they’re also more likely to raise blood pressure and cause nausea. SSRIs are gentler on the body but often leave people feeling emotionally flat.
Compared to older tricyclic antidepressants (TCAs), SNRIs are much safer. TCAs can cause dangerous heart rhythm changes, severe dry mouth, constipation, and urinary retention. SNRIs rarely cause those. That’s why TCAs are rarely used today unless nothing else works.
And then there’s tramadol - a painkiller that also acts as a weak SNRI. It’s not an antidepressant, but it’s sometimes used off-label for depression in chronic pain patients. The problem? It carries risks of addiction, respiratory depression, and seizures. It’s not a substitute for proper antidepressant treatment.
Who Benefits Most From SNRIs?
SNRIs aren’t for everyone. But they’re often the best choice if you have:
- Depression with chronic pain (nerve pain, back pain, fibromyalgia)
- Depression with fatigue or low energy
- Generalized anxiety or panic disorder
- Failed to respond to SSRIs
If you’re mostly struggling with sleep, appetite, or emotional numbness without physical symptoms, an SSRI might be a better starting point. If you have heart disease, uncontrolled high blood pressure, or a history of seizures, your doctor will be cautious with venlafaxine or levomilnacipran.
Real Talk: What Patients Say
On patient forums, the stories are mixed. One woman on Reddit said venlafaxine ‘gave her back her life’ - she went from bedridden to working full-time. Another said it made her feel like a ‘zombie’ and she quit after two weeks. Duloxetine users often say: ‘It helped my back pain more than my depression.’ Others say: ‘I lost weight at first, then gained 20 pounds.’
The common thread? SNRIs don’t make you ‘happy.’ They make you feel more like you did before depression took hold. For some, that’s enough. For others, it’s not. It’s not magic. It’s medicine. And it takes time - usually 4-6 weeks - to see real changes.
What’s Next for SNRIs?
Researchers are exploring new SNRIs with more balanced serotonin-norepinephrine effects to reduce side effects. One drug, LY03015, is in late-stage trials. There’s also growing interest in how SNRIs reduce inflammation in the brain - not just by changing neurotransmitters, but by calming overactive immune cells. This could explain why they help with pain and fatigue beyond just mood.
As the population ages, more people are living with both depression and chronic pain. SNRIs are filling a real gap. In 2022, they made up 32% of new antidepressant prescriptions in the U.S. Generic venlafaxine costs as little as $4 a month. Duloxetine, even after patent loss, still brings in over $1 billion in sales annually - proof that it works for people who need it.
SNRIs aren’t perfect. But for the right person, they’re one of the most powerful tools we have to treat depression - especially when it comes with pain, fatigue, or anxiety.
Can SNRIs cause weight gain?
Yes, but it’s complicated. Many people lose 5-7 pounds in the first few months, especially on duloxetine, due to reduced appetite and nausea. But after 6-12 months, weight gain often happens. This is likely due to improved mood leading to increased food intake and slower metabolism. It’s not the drug itself causing fat storage - it’s how your body responds over time.
How long until SNRIs start working?
Most people notice small improvements in energy and focus within 1-2 weeks. But full antidepressant effects - better mood, less anxiety, reduced pain - usually take 4-6 weeks. Some take up to 8 weeks. Don’t give up if you don’t feel better right away.
Are SNRIs addictive?
No, SNRIs are not addictive in the way opioids or benzodiazepines are. You won’t crave them or get high from them. But your body adapts to them. Stopping suddenly can cause severe withdrawal symptoms - brain zaps, nausea, dizziness - which is why tapering is essential. This is physical dependence, not addiction.
Can I drink alcohol while on SNRIs?
It’s not recommended. Alcohol can worsen dizziness, drowsiness, and liver stress. It can also make depression worse over time. Even one drink can increase side effects. If you choose to drink, limit it to very small amounts and never mix it with venlafaxine - it raises your risk of high blood pressure.
Do SNRIs help with anxiety?
Yes. Venlafaxine and duloxetine are both FDA-approved for generalized anxiety disorder, social anxiety, and panic disorder. Many patients report less rumination, fewer panic attacks, and improved ability to handle stress. The norepinephrine boost helps with the physical symptoms of anxiety - racing heart, trembling, tension.
What’s the difference between venlafaxine and duloxetine?
Venlafaxine has stronger effects on norepinephrine at higher doses and is better for anxiety disorders. Duloxetine is more balanced and is the go-to for nerve pain and fibromyalgia. Venlafaxine has a higher risk of blood pressure spikes and withdrawal symptoms. Duloxetine causes more nausea early on but is gentler on the heart. Which one you take depends on your main symptoms and health history.
Next Steps: What to Do If You’re Considering an SNRI
If you’re thinking about starting an SNRI:
- Keep a symptom journal for 2 weeks - track your mood, energy, sleep, and pain levels.
- Write down any medications, supplements, or herbs you take - especially painkillers or migraine meds.
- Ask your doctor about your blood pressure history and heart health.
- Start with the lowest effective dose and give it 6 weeks before deciding if it works.
- Plan your tapering strategy before you even start - this reduces the chance of withdrawal.
SNRIs can change your life. But they’re not a quick fix. They require patience, communication, and careful management. The goal isn’t to feel euphoric - it’s to feel steady. To wake up without dread. To move without pain. That’s worth working for.


SNRIs aren't magic. They're just chemical band-aids for a system that's been broken by capitalism, sleep deprivation, and the relentless pressure to be productive. You think your brain's 'imbalanced'? Nah. It's just responding rationally to a world that's designed to break people. The real question isn't why this drug works-it's why we need drugs at all.
bruh i took venlafaxine for 3 months and i swear my brain was doing zaps like a faulty wifi router 😵💫 no sleep, no appetite, just… static. i quit cold turkey cause i was done. now i just do yoga and drink matcha. who needs pharma when you got vibes?
Tommy, please don’t quit SNRIs cold turkey-it’s dangerous. Withdrawal symptoms like brain zaps are neurological, not psychological. A proper taper over 4–6 weeks, under medical supervision, reduces risk significantly. Many people recover fully with slow discontinuation. You’re not weak for needing help-you’re smart for seeking better info.
Man, I remember when I started duloxetine. First week? Nausea so bad I thought I was dying. Second week? Still nauseous but weirdly… awake? Like I could finally hear birds outside. Not happy. Not euphoric. Just… present. That’s the thing nobody tells you. SNRIs don’t fix your life. They just give you the bandwidth to fix it yourself. 🙏
While the pharmacological mechanisms of SNRIs are well-documented, it is imperative to acknowledge the profound psychosocial context in which these medications are prescribed. The over-reliance on pharmacological intervention in mental health care reflects systemic failures in access to therapy, economic stability, and community support. Medication is not a substitute for societal reform.
OMG YES!! 😭 I was on 60mg duloxetine for fibromyalgia and the first 2 weeks were hell-sweating like I was in a sauna, dry mouth like I’d eaten salt, and my cat kept staring at me like I was dying. But then? I walked 3 miles for the first time in 2 years. I cried. Not because I was sad. Because I felt my legs again. 💪❤️
SNRIs? LOL. Big Pharma's latest scam to keep you docile while they sell you more pills. You think your pain is 'neurological'? Nah. It's your soul screaming because you're trapped in a 9-5 drone world. They don't want you healed-they want you medicated. Check out the CIA's MKUltra files. Same playbook. 🧠💣
Key point: SNRIs modulate monoamine reuptake via SERT and NET inhibition → increased synaptic availability of 5-HT and NE → downstream neuroplasticity via BDNF upregulation. But clinically? The real win is functional restoration-not just mood, but movement, motivation, and meaning. If you're still fatigued after 6 weeks, it's not the drug-it's the dose or comorbidities. Time to titrate or switch.
I was skeptical too. Thought SSRIs were the only way. But after 4 years of chronic back pain and feeling like a ghost, duloxetine gave me back my mornings. Not perfect. Not a miracle. But I could get out of bed without crying. And that? That was everything.
So… you’re telling me we’ve spent 30 years telling people to ‘just take a pill’… and now we’re surprised they’re tired? 😏 Maybe if we stopped treating symptoms and started treating the fact that no one has time to breathe anymore… we wouldn’t need SNRIs. But hey, at least the stock prices are up.
Medication is a tool. Not a cure. Not a failure. Not a weakness. It is simply one part of healing. If you need it to get out of bed, to stop crying, to hold your child-then it is not a crutch. It is a bridge. And bridges are meant to be crossed. You are not broken. You are becoming.
SNRIs are overprescribed because doctors are lazy and patients want quick fixes. You think pain is neurological? Maybe you just need to stop being so soft. Get a job. Move more. Stop whining. This is America. You don't get medals for feeling bad. Just take a walk. Or don't. But don't blame the drug.