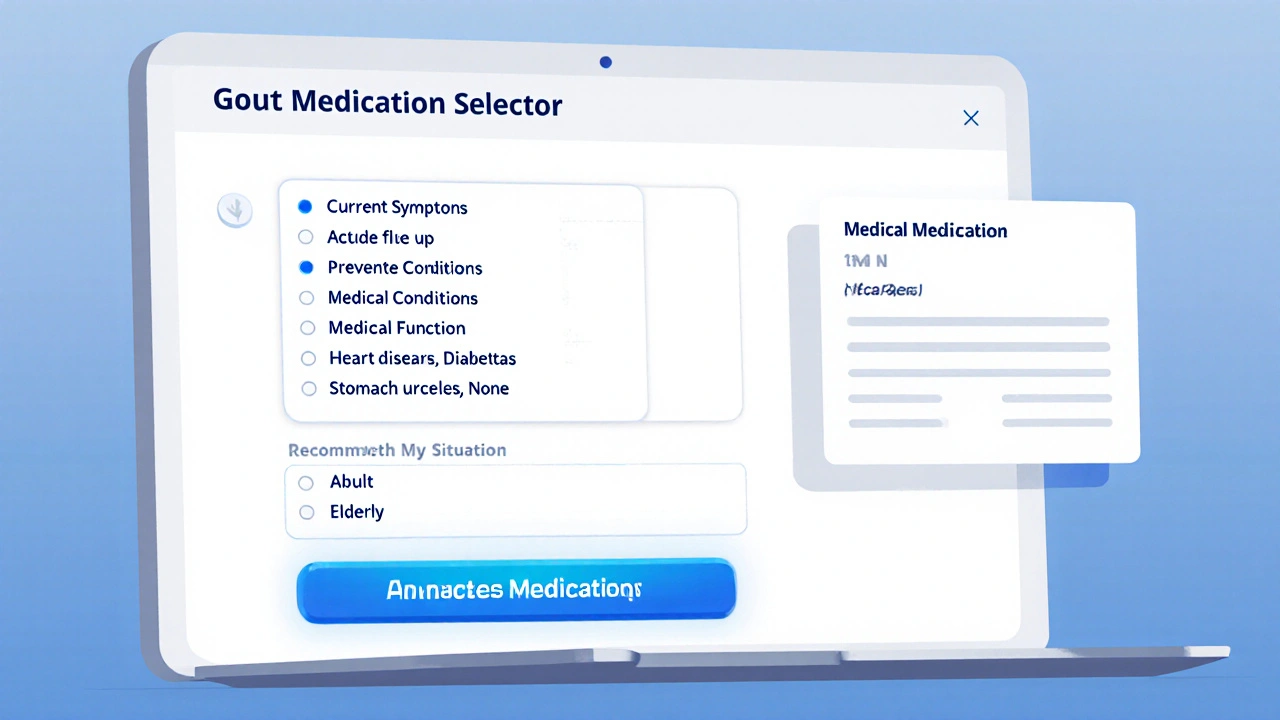
Gout Medication Selector
Recommended Medications
Enter your symptoms and medical information above to get personalized medication recommendations.
Medication Categories
Acute Attack Medications
For immediate pain relief during flares
Urate-Lowering Therapies
To prevent future flares by lowering uric acid
Combination Approach
Using multiple medication types
Key Takeaways
- Gout meds fall into two groups: drugs that stop attacks and drugs that prevent future flares.
- Allopurinol and febuxostat are first‑line urate‑lowering therapies for most patients.
- Colchicine, NSAIDs and corticosteroids act fast to ease pain during an acute flare.
- Kidney function, drug interactions and genetic factors shape which medication works best.
- Regular blood‑test monitoring and lifestyle tweaks boost long‑term success.
When dealing with gout, gout medications are drugs that lower uric acid levels or reduce inflammation during attacks are the cornerstone of management. Understanding how each class works, when to use it, and what side effects to watch for can turn a painful, unpredictable condition into something you control.
How Gout Happens: The Role of Uric Acid
Uric acid is a waste product formed when the body breaks down purines-found in foods like red meat, seafood and beer. Normally the kidneys filter it out, but if production outpaces excretion, blood levels rise (a state called hyperuricemia). Crystals then deposit in joints, especially the big toe, sparking sudden, excruciating inflammation known as a gout flare.
Two therapeutic goals emerge:
- Stop the inflammation now.
- Keep uric‑acid levels low enough to prevent future crystal formation.
Acute‑Attack Medications: Putting Out the Fire
When a flare strikes, you need fast relief. Three main drug families work within hours to days.
Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs)
Indomethacin is a potent NSAID commonly prescribed for gout attacks. It blocks prostaglandin production, easing pain and swelling. Typical dose: 50mg three times daily for 2‑5days. Watch for stomach upset, kidney strain and increased blood‑pressure risk.
Colchicine
Colchicine is an anti‑inflammatory derived from the autumn crocus. It interferes with neutrophil activation, which curtails crystal‑induced inflammation. A short‑course regimen (1.2mg then 0.6mg one hour later) works for most patients. High doses can cause diarrhea, nausea, and muscle pain, especially in those with kidney problems.
Corticosteroids
Prednisone is a systemic steroid that dampens the immune response. Oral doses of 30‑40mg daily, tapered over 1‑2weeks, are effective when NSAIDs or colchicine aren’t suitable (e.g., kidney disease, ulcer history). Side effects include blood‑sugar spikes, mood changes, and fluid retention.

Urate‑Lowering Therapies: Stopping Future Flare‑Ups
Once the pain subsides, the real work begins-keeping uric‑acid levels below 6mg/dL (or <6.5mg/dL in patients with kidney stones). Below are the most widely used long‑term options.
Allopurinol
Allopurinol is a xanthine oxidase inhibitor that decreases uric‑acid production. Starting dose is usually 100mg daily, titrated up to 300mg or more based on serum urate. Kidney function dictates the max dose. A rare but serious reaction-Allopurinol hypersensitivity syndrome-requires immediate stop and medical care.
Febuxostat
Febuxostat is a non‑purine xanthine oxidase inhibitor approved for patients who can’t tolerate allopurinol. Fixed doses of 40mg or 80mg daily achieve target urate levels quickly. Cardiovascular safety is under continued review, so discuss heart‑risk factors with your doctor.
Uricosuric Agents
These drugs increase renal excretion of uric acid.
- Probenecid blocks reabsorption of uric acid in the kidney tubules. Works best when kidney function is normal; dose is 250mg twice daily.
- Lesinurad is a newer uricosuric approved only in combination with a xanthine oxidase inhibitor. Adds 200mg daily to allopurinol or febuxostat for patients not reaching target urate.
Biologic Option: Pegloticase
Pegloticase is an intravenous enzyme that rapidly converts uric acid to allantoin, a harmless metabolite. Administered bi‑weekly, it’s reserved for refractory gout-cases that fail multiple oral agents. Infusion reactions and anti‑drug antibodies are common concerns.
Choosing the Right Regimen: Decision Factors
Picking a medication isn’t a one‑size‑fits‑all decision. Below is a quick decision matrix that matches patient characteristics with the most suitable drug class.
| Patient Profile | First‑Line Option | Alternative If Intolerant | Key Monitoring |
|---|---|---|---|
| Normal kidney function, no heart disease | Allopurinol | Febuxostat | Serum urate, liver enzymes |
| Kidney impairment (eGFR 30‑60mL/min) | Adjusted low‑dose Allopurinol | Febuxostat (preferred) | Renal panel, urate |
| History of severe rash to allopurinol | Febuxostat | Lesinurad+Febuxostat | Cardiac status, urate |
| Refractory gout despite oral therapy | Pegloticase | Combination uricosuric + xanthine oxidase inhibitor | Infusion reactions, urate |
Practical Tips to Maximize Success
- Start low, go slow: Titrate doses gradually to avoid sudden drops in uric acid that can trigger flares.
- Stay hydrated: Aim for at least 2L of water daily to help kidneys flush uric acid.
- Watch diet: Limit high‑purine foods (organ meats, anchovies) and sugary drinks.
- Monitor labs: Check serum urate every 2‑4weeks after dose changes, then quarterly.
- Adhere to schedule: Skipping doses can cause uric‑acid rebound, reigniting crystal formation.

Potential Pitfalls and How to Avoid Them
Even the best‑chosen drug can backfire if you overlook common issues.
- Drug interactions: Allopurinol can increase toxicity of azathioprine and cyclophosphamide. Inform your doctor about all prescriptions.
- Renal dosing errors: Over‑dosing a uricosuric in someone with low eGFR can cause kidney stones. Always adjust for kidney function.
- Missed flare prophylaxis: Starting urate‑lowering therapy without a short course of colchicine or NSAIDs can precipitate an acute attack. Use a “bridge” therapy for the first 3‑6months.
- Ignoring side‑effects: Early rash, fever, or unexplained fatigue may signal hypersensitivity; stop the drug and seek care immediately.
When to See a Healthcare Professional
Schedule a visit if you experience any of the following:
- Severe, persistent joint pain lasting more than 48hours despite OTC NSAIDs.
- Signs of infection (redness spreading, fever) after a flare.
- New kidney‑related symptoms: flank pain, blood in urine.
- Allergic‑type reactions: rash, swelling of lips or throat.
Early intervention can prevent joint damage and keep you moving.
Frequently Asked Questions
Can I take allopurinol during a gout flare?
Allopurinol does not relieve pain, and starting it during an active attack can actually worsen symptoms. Begin the drug after the flare subsides, and use colchicine or an NSAID as a bridge for the first few months.
Is febuxostat safe for people with heart disease?
Recent studies suggest a slightly higher risk of cardiovascular events with febuxostat compared to allopurinol, especially in patients with existing heart conditions. Discuss your cardiac history with a doctor before choosing febuxostat.
How often should I get blood tests while on gout medication?
Check serum urate 2‑4weeks after any dose change, then every 3‑6months once stable. Liver enzymes are monitored with allopurinol and febuxostat; kidney panels are essential for uricosurics.
Can diet alone control gout?
Diet helps lower uric‑acid spikes but rarely brings levels below treatment thresholds on its own. Combining dietary changes with medication yields the best long‑term control.
What should I do if I miss a dose of my urate‑lowering drug?
Take the missed dose as soon as you remember unless it’s almost time for the next one. Never double‑dose; a double hit can cause nausea or a sudden uric‑acid drop, which may trigger a flare.


Solid overview, thanks for the rundown.
When it comes to gout, the pharmacological playbook is anything but simple.
First off, the acute attack agents-NSAIDs, colchicine, and steroids-each carry a distinct mechanistic fingerprint.
Indomethacin, the classic NSAID, blitzes cyclooxygenase pathways delivering rapid pain relief, but it prowls the gastrointestinal lining like a tiger waiting to pounce.
Colchicine, harvested from the autumn crocus, hijacks neutrophil chemotaxis, and while a low‑dose regimen can be a lifesaver, the high‑dose version often leaves the patient with torrent‑like diarrhea.
Steroids, especially prednisone, act as the overarching immunosuppressant, perfect for patients where kidneys or ulcers make NSAIDs a no‑go.
Switching gears to urate‑lowering therapies, allopurinol has reigned supreme for decades, dampening xanthine oxidase and thus curbing uric acid production.
Yet febuxostat entered the arena promising greater potency, especially for those whose allopurinol dose hits a ceiling.
Both drugs demand vigilant monitoring of liver enzymes and renal function, because the price of over‑suppression can be a hidden minefield.
For the refractory gouturicist, pegloticase offers an injectable solution that enzymatically degrades uric acid, though infusion reactions can turn the tide against its use.
Lifestyle tweaks-cutting back on purine‑rich foods, moderating alcohol, and maintaining hydration-are the unsung heroes that amplify pharmacotherapy.
Kidney function is the litmus test for choosing between colchicine and NSAIDs, as diminished clearance can turn a therapeutic ally into a toxic adversary.
Patients with cardiovascular comorbidities must steer clear of certain NSAIDs that may exacerbate blood pressure, a nuance often glossed over in quick‑fire prescriptions.
Genetic polymorphisms, especially in the HLA‑B*58:01 allele, predispose some ethnic groups to severe allopurinol hypersensitivity, underscoring the need for personalized medicine.
The bottom line is that gout management demands a tailored algorithm, not a one‑size‑fits‑all script.
Every clinician should wield a decision tree that weighs acute pain, chronic uricemia, organ function, and patient preference before committing to a regimen.
Only then can we turn the erratic flare‑ups into manageable chapters of a patient’s health narrative.
Thanks for the deep dive-feels like you just mapped the whole galaxy of gout meds. 🌌
While the science is solid, I keep thinking about how every flare is a reminder that our bodies are constantly negotiating with the environment. 🍃
Balancing the chemical cascade with lifestyle choices is almost like a meditation practice, a dance between intention and biology. 🙏
Appreciate the clear split between acute and preventive options.
Look, I get that gout meds are a maze, but honestly the article could’ve cut some of the fluff.
People want straight facts: which pill works fast, which one you can stay on for life, and what to watch out for.
All that talk about crystals and purines is nice for a lecture, not so much for someone clutching their big toe at 2 am.
Still, the breakdown of NSAIDs versus colchicine was helpful, and the reminder about kidney checks is spot on.
If they added a quick table, it’d be perfect for the layperson.
Yo the guide is decent but it misses the mark on dosage warnings – people skip the fine print and end up in the ER.
Also, the allopurinol side effects section could be more upfront about the rash risk – it’s scary.
Gotta be real about how aggressive the meds can get if misused.
Great info keep it up
Wow, this article really tries to be exhaustive, but it’s painfully obvious the author thinks they’re the ultimate authority on gout.
The dramatics about crystals and “erratic flare‑ups” read like a thriller novel, not a medical guide.
Let’s be real: most patients just want a pill that stops the pain, not a lecture on HLA‑B*58:01.
Nice breakdown of the medication categories.
If you’re new to this, remember to talk to your doctor about kidney function before starting colchicine.
Also, staying hydrated can really help keep uric acid levels down.
Hey folks, just wanted to add that if you’re on allopurinol, keep an eye on your liver enzymes – I learned that the hard way 😊
Also, don’t forget to pace yourself with alcohol; even a light beer can stir up a flare.
In many cultures, dietary habits play a huge role – spices, legumes, and traditional dishes can affect uric acid.
When you discuss meds with your doctor, bring up any herbal supplements you take; they can interact with urate‑lowering drugs.
Honestly, the mainstream medical community hides the truth about pharmaceutical influence.
They’ll push allopurinol because it’s cheap, while newer, possibly safer options get buried.
Read between the lines and don’t accept the curated narrative at face value.
The so‑called "guidelines" are just a cover‑up for big pharma agendas.
If you’re smart, you’ll question every recommendation and look for independent studies.
Don’t let them dictate your health choices.
This article does a decent job of laying out the basics, but a bit more nuance on drug interactions would be helpful.
For example, NSAIDs can affect blood pressure meds, which is important for older patients.
While the piece is thorough, it completely ignores the emerging role of lifestyle‑first protocols that can sometimes replace meds altogether.
Why are we still glorifying pills when diet, exercise, and stress management have shown promising results?
Time to rethink the pharmaceutical monopoly on gout therapy.