Anticoagulant-COVID-19 Treatment Interaction Checker
Anticoagulant Management During COVID-19
Get personalized guidance based on your specific medications and treatment plan
When you're on a blood thinner-whether it's warfarin, apixaban, or rivaroxaban-and you get a serious respiratory infection like COVID-19, your treatment becomes a tightrope walk. One wrong move with your meds can lead to dangerous bleeding or a life-threatening clot. This isn't theoretical. During the pandemic, hospitals saw a spike in patients who bled after taking their usual anticoagulant dose while on antiviral drugs like Paxlovid. Others developed clots because their blood thinner stopped working as expected. The science behind this is complex, but the practical impact is simple: anticoagulant interactions with COVID-19 treatments can kill if not managed right.
Why COVID-19 Makes Blood Thinner Management So Risky
COVID-19 doesn't just attack your lungs. It triggers your body to go into overdrive, producing inflammatory signals that make your blood stickier than normal. This is called a hypercoagulable state. In severe cases, tiny clots form in the lungs' smallest blood vessels, blocking oxygen flow. Studies show these microclots are present in about 70% of critically ill patients. That's why doctors started giving therapeutic doses of blood thinners to hospitalized patients-not just low-dose预防, but full treatment doses-to keep clots from forming. But here's the catch: the same drugs used to treat COVID-19 can mess with how your blood thinner works. Some boost its effect. Others turn it off. And both outcomes are dangerous.How Paxlovid and Other Antivirals Interfere with Blood Thinners
Paxlovid, the most widely used antiviral for early COVID-19, contains two drugs: nirmatrelvir and ritonavir. Ritonavir is the problem. It's a powerful inhibitor of CYP3A4 and P-glycoprotein-two systems your liver and gut use to break down and remove drugs like apixaban, rivaroxaban, and dabigatran. When ritonavir blocks these systems, your blood thinner builds up in your bloodstream. A 2022 study of 12 patients on DOACs who got Paxlovid showed their anticoagulant levels jumped by 3 to 5 times. That's not a small change. That's enough to cause major bleeding. One Reddit user shared a case where a patient on rivaroxaban ended up in the ER with gastrointestinal bleeding after continuing his full dose during Paxlovid treatment. He needed two units of blood. On the flip side, dexamethasone-a steroid used in severe COVID-19-does the opposite. It speeds up how fast your body clears DOACs. Research shows it can reduce their effect by up to 50%. That means a patient might be getting what feels like a normal dose, but their blood thinner isn't working at all. That's when clots form.Warfarin vs. DOACs: Different Problems, Same Danger
Warfarin doesn't rely on CYP3A4 the way DOACs do. Instead, it's affected by changes in vitamin K levels and liver function. But that doesn't make it safer. During the pandemic, many patients on warfarin saw their INR (a measure of blood clotting time) spike unexpectedly when they started azvudine or other antivirals. One case report described a 70-year-old man whose INR jumped from 2.5 to 3.2 after adding dexamethasone and azvudine to his regimen. That put him at higher risk for bleeding. The big advantage of warfarin is that we can measure its effect with a simple blood test. DOACs don't have a routine monitoring test. That means you can't tell if your drug level is too high or too low unless you get a special test-something most clinics don't do on a daily basis. So if you're on a DOAC and get COVID-19, you're flying blind.What Doctors Actually Do in Real Cases
There's no one-size-fits-all answer. The best approach depends on your risk for clots versus your risk for bleeding. For patients with a high clot risk-like someone with atrial fibrillation and a CHA2DS2-VASc score of 4 or higher-doctors often stop the DOAC entirely during the 5-day Paxlovid course. They replace it with daily injections of enoxaparin (Lovenox), which doesn't interact with Paxlovid. After Paxlovid ends, they restart the DOAC two days later. For lower-risk patients, some guidelines suggest holding the DOAC for the full 5 days and restarting without bridging. But if you're already on therapeutic anticoagulation for a recent clot, stopping even for 5 days can be risky. That's why many hospitals now use a risk calculator to decide. Dabigatran is tricky. In the U.S., guidelines say to avoid it entirely with Paxlovid if your kidney function is between 15 and 30 mL/min. In Europe, they allow it with a dose cut to 75 mg twice daily, as long as you space it 12 hours apart from Paxlovid. That kind of inconsistency confuses patients and pharmacists alike.What You Should Know If You're on a Blood Thinner
If you're on a blood thinner and get COVID-19, here's what you need to do right away:- Call your doctor or pharmacist before taking any new medication-even over-the-counter ones.
- Tell them exactly which blood thinner you're on and your kidney function (if you know it).
- Don't stop or change your dose without professional advice.
- Watch for signs of bleeding: unusual bruising, nosebleeds that won't stop, dark or bloody stools, vomiting blood, severe headaches.
- Watch for signs of clotting: sudden shortness of breath, chest pain, swelling or pain in one leg, confusion or slurred speech.
Where to Find Reliable, Updated Information
The rules change fast. What was safe last year might be dangerous now. That's why you need to check real-time resources:- The Liverpool COVID-19 Drug Interactions website updates daily and has tracked over 1.2 million queries since 2020. It's free, easy to use, and trusted by hospitals worldwide.
- The FDA's Drug Development and Drug Interactions Table lists 287 medications with specific guidance on anticoagulant interactions.
- Your pharmacist can access the same tools. Don't be shy about asking them to double-check your meds.
What's Changing in the Near Future
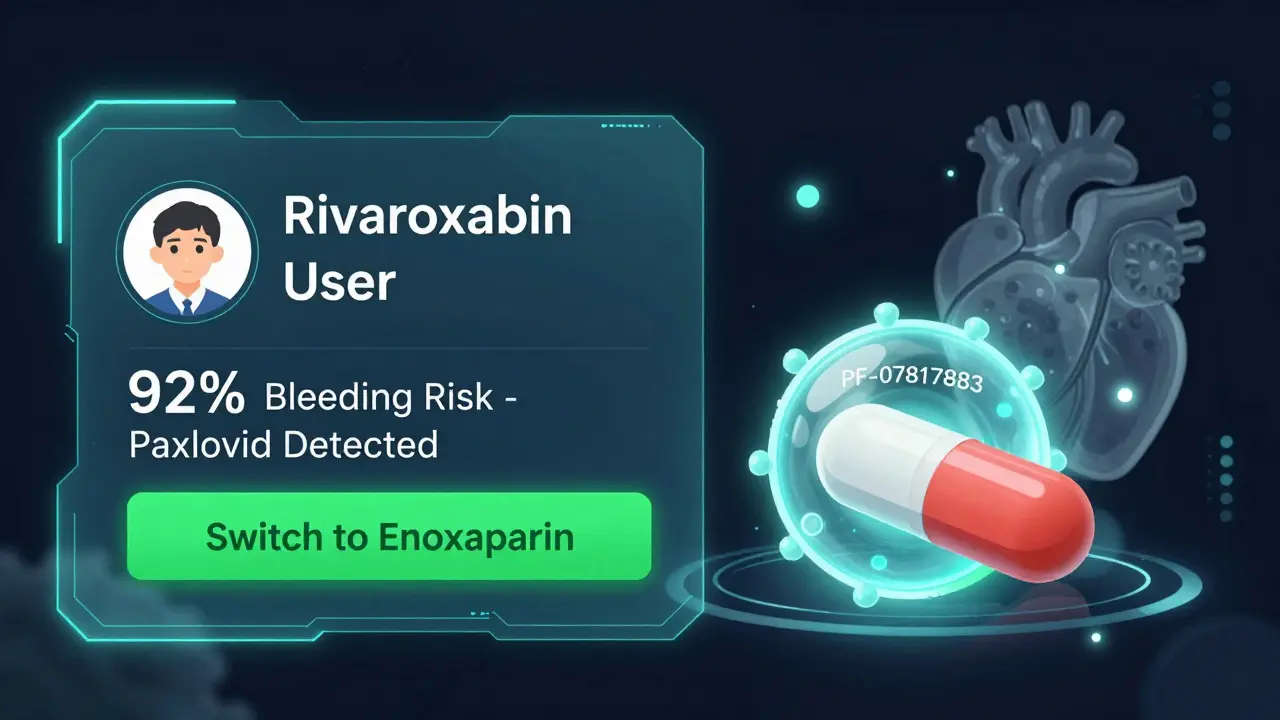
The good news? The pharmaceutical industry is listening. Pfizer is testing a next-generation antiviral, PF-07817883, that doesn't inhibit CYP3A4. Early data suggests it won't interfere with blood thinners at all. If it works, it could eliminate the biggest problem in this space. Also, new tools are emerging. A 2023 study in Nature Medicine showed a machine learning model could predict interaction severity with 89.4% accuracy using just 12 patient factors. That means in the future, your doctor might get an automated alert: "This patient on rivaroxaban has 92% risk of bleeding if given Paxlovid. Recommend switch to enoxaparin." For now, though, the responsibility falls on you and your care team. Don't assume your doctor knows every interaction. Don't assume your pharmacist will catch it unless you tell them you're on a blood thinner. And never, ever take a new COVID-19 treatment without checking.Can I keep taking my blood thinner if I get COVID-19?
It depends on your specific situation. If you're on warfarin, your doctor will likely monitor your INR more closely and adjust your dose. If you're on a DOAC like apixaban or rivaroxaban, you may need to stop it during Paxlovid treatment and use a different anticoagulant temporarily. Never stop or change your dose without medical advice.
Is it safe to take ibuprofen or acetaminophen with blood thinners during COVID-19?
Acetaminophen (Tylenol) is generally safe with blood thinners. Ibuprofen and other NSAIDs can increase bleeding risk, especially in people with kidney issues or those on high-dose anticoagulants. Use acetaminophen first unless your doctor says otherwise.
How long does the risk last after COVID-19?
The hypercoagulable state can last for weeks after recovery. Studies show 65% of patients still have elevated D-dimer levels (a clotting marker) 14 to 21 days after discharge. That's why many doctors recommend continuing therapeutic anticoagulation for at least 7 days after leaving the hospital-even if you feel better.
What if I can't get my DOAC levels checked?
Most clinics don't routinely test DOAC levels. If you're on a DOAC and get sick with COVID-19, your doctor will rely on your kidney function, age, weight, and other risk factors to decide whether to stop, reduce, or switch your medication. If you're at high risk for clots, they may use enoxaparin injections instead.
Are there any new antivirals that don't interact with blood thinners?
Yes. Pfizer is developing a new antiviral, PF-07817883, currently in Phase 2 trials, that doesn't inhibit CYP3A4. Early results suggest it won't interfere with DOACs or warfarin. If approved, it could replace Paxlovid for many patients on blood thinners.
What to Do Next
If you're on a blood thinner and have a respiratory infection:- Don't wait. Contact your prescriber or pharmacist immediately.
- Have your medication list ready, including doses and kidney function if known.
- Ask: "Should I stop my blood thinner during this treatment?" and "What should I use instead?"
- Keep a log of any unusual symptoms-bruising, bleeding, shortness of breath, leg pain.
- Use the Liverpool website to check interactions yourself before your appointment.


So let me get this straight-Paxlovid’s ritonavir is basically a molecular bulldozer that smashes your liver’s ability to clear DOACs? That’s not a drug interaction, that’s a full-on biochemical hostage situation. And we’re just supposed to wing it with enoxaparin injections while hoping the clots don’t sneak up on us? This isn’t medicine, it’s high-stakes Russian roulette with a prescription pad.
There’s a deeper epistemological problem here: we treat anticoagulants like on/off switches when they’re actually dynamic, system-wide modulators. The body doesn’t care about drug labels-it responds to flux. When you introduce ritonavir, you’re not just altering pharmacokinetics-you’re destabilizing an entire hemostatic equilibrium. We need systems biology, not just algorithmic dosing charts. The fact that we’re still relying on INR for warfarin while DOACs are black boxes? That’s not clinical practice. That’s medical colonialism.
Of course the pharmaceutical industry is pushing this. They don’t want you to know that the real solution is stopping anticoagulants altogether-no more bleeding, no more lawsuits. The ‘risk calculator’? A distraction. The real risk is trusting a system that profits from your confusion. They’ll sell you a new antiviral next year that ‘doesn’t interact’-while quietly adding another 12 drugs to the interaction list. Wake up.
My cousin in Mumbai got COVID last year on apixaban-doctor told him to pause it for 5 days, switch to daily Lovenox shots. He cried every time he gave himself the injection-but he’s alive today. No bleeding. No clots. Just discipline, and a pharmacist who actually called him back. This isn’t rocket science. It’s care. And care means listening, not just clicking on a website.
Why is the U.S. still letting foreign drug protocols dictate our care?! Europe lets people take dabigatran with Paxlovid at 75mg? That’s reckless! We have the best medical minds on Earth-and we’re following some EU guideline because it sounds nice?! No. We need American standards. American oversight. American solutions. Not some diluted, watered-down, international compromise that gets people killed!
Just had a patient on rivaroxaban come in with a nosebleed that wouldn’t stop after Paxlovid. We switched to enoxaparin, did a quick DOAC level (thank god the lab was open), and it was 4x normal. He’s fine now. But here’s the thing-no one asked him if he’d taken his meds on time. No one asked if he’d been drinking grapefruit juice. We focus on the drugs, not the person. Please, if you’re on a blood thinner, bring your pill bottles to every appointment. Even the OTC stuff. Even the turmeric capsules. I’m not joking.
The data on hypercoagulability persisting beyond acute infection is compelling. D-dimer elevation at 14–21 days post-discharge suggests a prolonged prothrombotic state that current guidelines inadequately address. We must consider extended therapeutic anticoagulation in high-risk populations, even in the absence of overt symptoms. This is not over-treatment-it is anticipatory risk mitigation grounded in pathophysiology. The burden of proof should lie with those advocating for early cessation, not continuation.
EVERYONE knows the government and Big Pharma are hiding the truth. Paxlovid doesn’t cause bleeding-it’s the microchips in the pills that make your blood thin. They’ve been testing this since 2019. That’s why they pushed it so hard during the pandemic. The ‘CYP3A4 inhibition’? A cover story. The real danger is the nanotech in the ritonavir that syncs with your phone’s 5G signal and triggers clotting when you’re near a cell tower. That’s why your leg swells after watching the news. That’s why your INR goes wild when you use Wi-Fi. Don’t take the pill. Don’t trust the hospital. Get your blood tested by a naturopath. And unplug everything. EVERYTHING.
Just a quick note: if you’re on a blood thinner and get sick, don’t panic. Just call your pharmacist. Seriously. They’re the unsung heroes here. They know the interactions better than most docs, and they’ll take the time to explain it without jargon. I’ve seen it a hundred times-someone comes in terrified, they walk out calm. It’s not magic. It’s just someone who cares enough to look it up.