When two drugs are taken together, they don’t just sit side by side in your body. They talk to each other-sometimes helping, sometimes hurting. This isn’t about one drug changing how the other is absorbed or broken down. That’s pharmacokinetics. This is about what happens at the receptor level, where drugs actually do their job. This is pharmacodynamic interaction: when one drug changes how another drug works, even if their concentrations stay exactly the same.
How Drugs Talk at the Receptor Level
Every drug has a target-usually a receptor on a cell. Think of it like a key fitting into a lock. Some drugs are keys that turn the lock to open a door (like activating a receptor). Others block the lock so no other key can turn it. When two drugs go after the same lock, things get messy. Take albuterol and propranolol. Albuterol opens airways by activating beta-2 receptors in the lungs. Propranolol blocks those same receptors to slow the heart. If someone with asthma takes both, propranolol can shut down albuterol’s effect completely. The albuterol is still in the bloodstream at the same level-it just can’t reach its target. That’s receptor competition. The drug with higher affinity wins. Propranolol’s affinity for beta receptors is often 10 to 100 times stronger than albuterol’s. That’s why even small doses can cause trouble. It’s not just about blocking. Sometimes drugs team up. Trimethoprim and sulfamethoxazole work together like a two-step lockpick. One blocks an early step in bacterial folic acid production; the other blocks the next step. Together, they’re far more powerful than either alone. In fact, their combined effect lets doctors use 75% less of each drug than if they were given separately. That’s synergy-and it’s intentional.The Three Types of Pharmacodynamic Interactions
There are three main ways drugs interact at the level of effect:- Additive: The total effect equals the sum of each drug’s individual effect. Like taking two painkillers that both work on the same pathway-acetaminophen and codeine. Together, they give you more pain relief than either alone, but not more than you’d expect.
- Synergistic: The combined effect is stronger than the sum. Think of antibiotics like vancomycin and gentamicin used together against serious infections. They attack bacteria in different ways, and together, they kill faster and more completely than either could alone.
- Antagonistic: One drug reduces or cancels out the effect of another. This is the most dangerous type. NSAIDs like ibuprofen can block the blood pressure-lowering effect of ACE inhibitors by reducing kidney blood flow. In one study, this interaction cut renal blood flow by about 25% in hypertensive patients. That’s not just a tweak-it can make the blood pressure medication useless.
The Most Dangerous Combinations
Some drug pairs are like walking into a minefield. Even experienced clinicians get caught. One of the most feared is combining SSRIs (like sertraline or fluoxetine) with MAOIs (like phenelzine). Both increase serotonin levels. Together, they can trigger serotonin syndrome-a potentially fatal condition with high fever, muscle rigidity, confusion, and seizures. A 2021 meta-analysis found this combination increases serotonin syndrome risk by 24 times. It doesn’t take a high dose. Sometimes, just starting an SSRI while still on an MAOI is enough. Another deadly combo: opioids and opioid antagonists. If someone is physically dependent on morphine or oxycodone and gets naloxone (to reverse an overdose), they can go into sudden, violent withdrawal-seizures, vomiting, panic attacks. It’s not the overdose being reversed. It’s the body being yanked off its drug. Even common OTC drugs can cause trouble. NSAIDs and blood thinners like warfarin don’t just add up-they multiply bleeding risk. A 2022 UK drug safety report found that NSAID use with anticoagulants was involved in over 40% of serious gastrointestinal bleeds in elderly patients.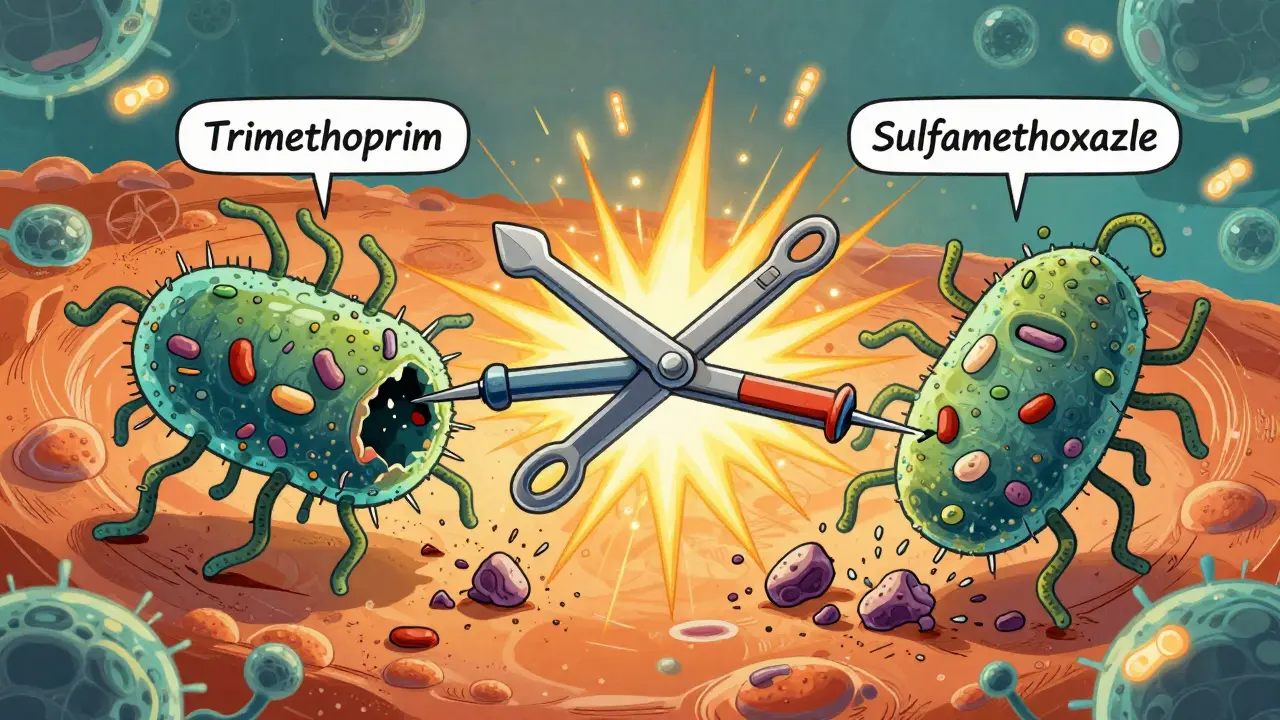
When Interactions Are Helpful
Not all pharmacodynamic interactions are bad. Medicine uses them on purpose. Low-dose naltrexone (LDN), originally an opioid blocker, is now being used with antidepressants to treat treatment-resistant depression. In a 12-week trial with 142 patients, 68% saw improvement with LDN plus an antidepressant, compared to just 42% on the antidepressant alone. The theory? Naltrexone briefly blocks opioid receptors, causing the body to ramp up natural endorphin production-which seems to boost mood regulation. Another example: combining diuretics with ACE inhibitors. Diuretics lower blood pressure by flushing out fluid. ACE inhibitors relax blood vessels. Together, they’re more effective than either alone-and often allow lower doses of each, reducing side effects like dizziness or electrolyte imbalances.Why These Interactions Are Hard to Spot
Unlike pharmacokinetic interactions-where you can adjust a dose based on liver enzyme activity-pharmacodynamic interactions are invisible to standard blood tests. You can’t measure the interaction. You can only see its result: a patient’s blood pressure didn’t drop, their asthma worsened, or they collapsed with serotonin syndrome. A 2022 survey of over 1,200 doctors found that 63% ran into a dangerous pharmacodynamic interaction at least once a month. The top culprits? Anticoagulants with antiplatelets (38% of cases) and multiple CNS depressants like benzodiazepines, opioids, and sleep aids (29%). Electronic health record systems flag many interactions-but they miss nearly a quarter of the serious ones. Why? Because many algorithms only look for known, high-risk pairs. They don’t account for subtle physiological changes. For example, a system might not warn you that an NSAID taken with a diuretic could worsen kidney function in someone with borderline renal function. That’s a pharmacodynamic interaction masked as a kidney issue.
Who’s Most at Risk?
Older adults are the most vulnerable. On average, people over 65 take 4.8 prescription medications. That’s not just a number-it’s a recipe for interaction. A 2021 review in BMJ Quality & Safety showed that pharmacist-led medication reviews cut adverse events from pharmacodynamic interactions by 58% in elderly patients. The most common preventable event? NSAIDs combined with antihypertensives. That’s something a pharmacist can catch in five minutes by asking, “Are you still taking ibuprofen for your arthritis?” People with narrow therapeutic index drugs are also at higher risk. These are medications where the difference between a helpful dose and a toxic one is tiny. Think warfarin, digoxin, lithium, or phenytoin. A small change in effect-like an NSAID reducing kidney clearance of lithium-can push levels into the danger zone. In fact, 83% of life-threatening pharmacodynamic interactions involve at least one drug with a therapeutic index under 3.0.What You Can Do
If you’re a patient:- Keep a written list of every medication you take-including supplements, OTC drugs, and herbal products.
- Ask your pharmacist: “Could any of these interact in a way that makes one less effective-or more dangerous?”
- Don’t assume “natural” means safe. St. John’s wort can block the effect of birth control, antidepressants, and even some heart medications.
- Know your receptor targets. Understand whether a drug is an agonist, antagonist, or partial agonist.
- Pay attention to drugs with narrow therapeutic windows.
- Use tools like the University of Liverpool’s HIV Drug Interactions Database-even if you’re not treating HIV. It’s one of the most comprehensive public resources.
- When in doubt, check the dose-response curve. If a drug’s effect plateaus quickly, adding another drug won’t help much-but it might increase risk.
The Future of Managing Interactions
The field is moving fast. The FDA now requires pharmacodynamic interaction studies for all new CNS drugs. The European Medicines Agency reports that 34% of new drug applications now include these studies-up from 19% in 2015. Researchers are building smarter tools. Dr. Rada Savic’s team at UCSF created a machine learning model that predicts serotonin syndrome risk with 89% accuracy by analyzing polypharmacy patterns. The UK’s NHS is piloting real-time alerts in electronic records that flag dangerous combinations before the prescription is even filled. But technology alone won’t fix this. The biggest predictor of safety? A clinician who understands not just what drugs do-but how they talk to each other.What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions change how the body handles the drug-like speeding up its breakdown or blocking its absorption. Pharmacodynamic interactions happen at the target site, like receptors or cells. The drug levels stay the same, but the effect changes because one drug alters how another works at its site of action.
Can over-the-counter drugs cause serious pharmacodynamic interactions?
Yes. Common OTC drugs like ibuprofen, naproxen, and even antihistamines can interfere with prescription medications. Ibuprofen can block the effect of blood pressure drugs like lisinopril. Diphenhydramine (Benadryl) can add to the sedation of opioids or benzodiazepines, increasing fall risk in older adults. Even herbal supplements like St. John’s wort can reduce the effectiveness of antidepressants and birth control pills.
Why are pharmacodynamic interactions harder to detect than pharmacokinetic ones?
Blood tests show drug concentrations, but they can’t show how drugs are affecting receptors or physiological pathways. A patient might have perfect levels of their blood pressure medication, yet their pressure remains high because an NSAID is blocking its effect. That’s invisible to lab tests-only clinical observation catches it.
Are there any safe combinations of drugs that work better together?
Absolutely. Trimethoprim and sulfamethoxazole work together to kill bacteria more effectively than either alone. Low-dose naltrexone combined with antidepressants has shown improved results in treatment-resistant depression. Some heart failure patients benefit from combining beta-blockers with ACE inhibitors because they target different parts of the disease process. These are intentional, evidence-based synergies.
How can I reduce my risk of harmful drug interactions?
Keep a full, updated list of all medications and supplements you take. Bring it to every appointment. Ask your pharmacist to review it every time you get a new prescription. Don’t start new OTC drugs or supplements without checking with a professional. If you notice sudden changes-like dizziness, confusion, or worsening symptoms-ask whether a new drug might be interfering with an old one.


Man, I had no idea my ibuprofen could be silently sabotaging my blood pressure med. I’ve been popping those like candy for my back pain. Guess I’m scheduling a pharmacist chat this week.
Also, St. John’s wort? That stuff’s basically a sneaky traitor in my supplement drawer. Who knew ‘natural’ meant ‘dangerous combo’?
This is 🔥! I’m a med student in India and this breakdown made so much sense. The receptor lock analogy? Perfect. I’ll be sharing this with my study group.
Also, the part about trimethoprim-sulfamethoxazole synergy? We use that combo daily for UTIs. Never thought about it like a two-step lockpick. Mind blown 🤯
So let me get this straight - my body’s basically a high school hallway where drugs are kids shoving each other for the same locker? And sometimes they team up to bully the other kids?
Also, serotonin syndrome? That’s not a side effect, that’s a horror movie plot. I’m now terrified of my own antidepressant and my neighbor’s CBD gummies.
Also also - why do we even make drugs that talk to each other? Can’t we just give people one magic pill? 🙃
Pharmacodynamic interactions are the silent killers. No lab test catches them. Just a patient who says, ‘I feel weird.’
I’ve seen it. A 72-year-old on warfarin starts taking ibuprofen for knee pain. Two weeks later, she’s in the ER with a GI bleed. No one asked about the OTC stuff.
Pharmacists are the unsung heroes here.
Guys, this is why we need better systems - and why we need to stop treating patients like data points.
I’ve been a nurse for 18 years. I’ve seen people die because someone thought, ‘Oh, it’s just Advil.’ It’s not. It’s a silent grenade in their bloodstream.
But here’s the good news: we can fix this. Ask the questions. Listen to the patient. Check the list. It’s not complicated. It’s just not prioritized.
Let’s make pharmacodynamic safety part of every visit. Not an afterthought. Not a checkbox. A habit.
the part about ldn and antidepressants is so cool i had no idea naltrexone could do that. i thought it was just for opioid overdoses. wow. i’m gonna look into this for my cousin who’s been stuck in depression for years.
Esteemed colleagues, I must express my profound appreciation for the meticulous elucidation of pharmacodynamic principles presented herein. The analogical framework of receptor-level interactions, particularly the lock-and-key paradigm, constitutes an exemplary pedagogical tool, facilitating comprehension among both novices and seasoned practitioners.
Moreover, the statistical corroboration provided - particularly the 24-fold increase in serotonin syndrome risk - is not merely informative, but morally imperative for clinical vigilance.
Let us not forget: the human body is not a pharmacological vending machine. It is a symphony of delicate, interdependent systems. One misplaced note - a single NSAID - can silence the entire orchestra.
That study about pharmacists cutting adverse events by 58%? That’s the real MVP stat. Why aren’t we funding more pharmacist-led reviews? They’re cheaper than ER visits and way more effective.
Also, I’ve had patients tell me they ‘don’t count’ supplements because they’re ‘natural.’ I just nod and think, ‘You’re basically drinking liquid chaos.’
Can we make pharmacists mandatory for every med refill? Just asking.
so like… if my blood pressure med stops working after i start taking tylenol, is that the interaction? or is it just my meds being weak?
Oh wow. So this is why my uncle collapsed after taking ibuprofen with his blood pressure pills. And now everyone’s acting like it’s his fault for being ‘old’ and ‘forgetful.’
It’s not his fault. It’s the system’s fault. Doctors don’t ask. Pharmacies don’t warn. The FDA doesn’t care until someone dies.
And now you’re all acting like this is some deep scientific mystery. No. It’s negligence dressed up as medicine.
You know, back home in Nigeria, we say: ‘The medicine that heals you can also bury you.’
This post? It’s like someone took that old saying and turned it into a science textbook. I read this and I thought - we’re all walking around with invisible wires in our bodies, and someone’s pulling them without asking.
Maybe the real cure isn’t more drugs. Maybe it’s more listening. To the patient. To the pharmacist. To the silence between the pills.