Antibiotic Decision Tool
Antibiotic Decision Tool
This tool helps identify the most appropriate antibiotic alternative based on your specific infection and health factors. Select your options below to see recommendations.
Recommendation
Mikacin Injection is a brand name for amikacin, a powerful antibiotic used to treat serious bacterial infections. It’s often chosen when other antibiotics fail, especially in hospital settings. But it’s not the only option. If you’re wondering whether Mikacin is the right choice-or if there’s something better-you’re not alone. Many patients and even some doctors weigh the pros and cons of amikacin against other antibiotics before making a decision.
What is Mikacin Injection (Amikacin)?
Mikacin Injection is a brand-name version of amikacin, an aminoglycoside antibiotic that kills bacteria by disrupting their ability to make proteins. It was first developed in the 1970s and remains one of the most effective tools against resistant strains of Gram-negative bacteria like E. coli, Pseudomonas, and Klebsiella.
Amikacin is typically given by injection or IV, often in hospitals or clinics. It’s not taken orally because it doesn’t absorb well through the gut. Doctors usually turn to it when first-line antibiotics like penicillin or cephalosporins don’t work-or when the infection is life-threatening.
It’s not gentle. Amikacin can damage the kidneys and hearing, especially with long-term use or in older adults. That’s why it’s reserved for serious cases. Blood tests are often done to monitor kidney function and drug levels during treatment.
Why Consider Alternatives to Mikacin?
Not every infection needs amikacin. Many doctors avoid it unless absolutely necessary because of its side effects. The goal isn’t just to kill bacteria-it’s to do it safely. That’s where alternatives come in.
Some infections respond better to other drugs. Others can be treated with newer antibiotics that have fewer risks. Cost, availability, and patient history (like past kidney problems or hearing loss) also play a role.
Here’s what you need to know about the most common alternatives to Mikacin Injection.
Gentamicin: The Classic Alternative
Gentamicin is another aminoglycoside antibiotic, similar to amikacin but older and less expensive. It’s widely used around the world and often the first choice for severe Gram-negative infections.
Both drugs work the same way. But gentamicin is more likely to cause kidney damage and hearing loss than amikacin in some studies. However, it’s still very effective against many common hospital-acquired infections.
One key difference: amikacin works better against certain resistant strains. If a bacteria has become resistant to gentamicin, amikacin might still kill it. That’s why many labs test for resistance patterns before choosing between them.
In practice, many hospitals start with gentamicin because it’s cheaper. If the infection doesn’t improve in 48 hours, they switch to amikacin.
Tobramycin: The Pseudomonas Specialist
Tobramycin is an aminoglycoside that’s especially strong against Pseudomonas aeruginosa, a tough bacterium that causes lung infections in cystic fibrosis patients and hospital-acquired pneumonia.
Studies show tobramycin is slightly more effective than amikacin against Pseudomonas. That’s why it’s often preferred for lung infections in people with cystic fibrosis. In fact, inhaled tobramycin is a standard maintenance treatment for these patients.
Like amikacin, tobramycin carries risks to the kidneys and hearing. But it’s often better tolerated in short-term use. It’s also available in inhalation form, which amikacin is not.
If you’re being treated for a lung infection caused by Pseudomonas, your doctor may lean toward tobramycin-even if you’ve tried amikacin before.
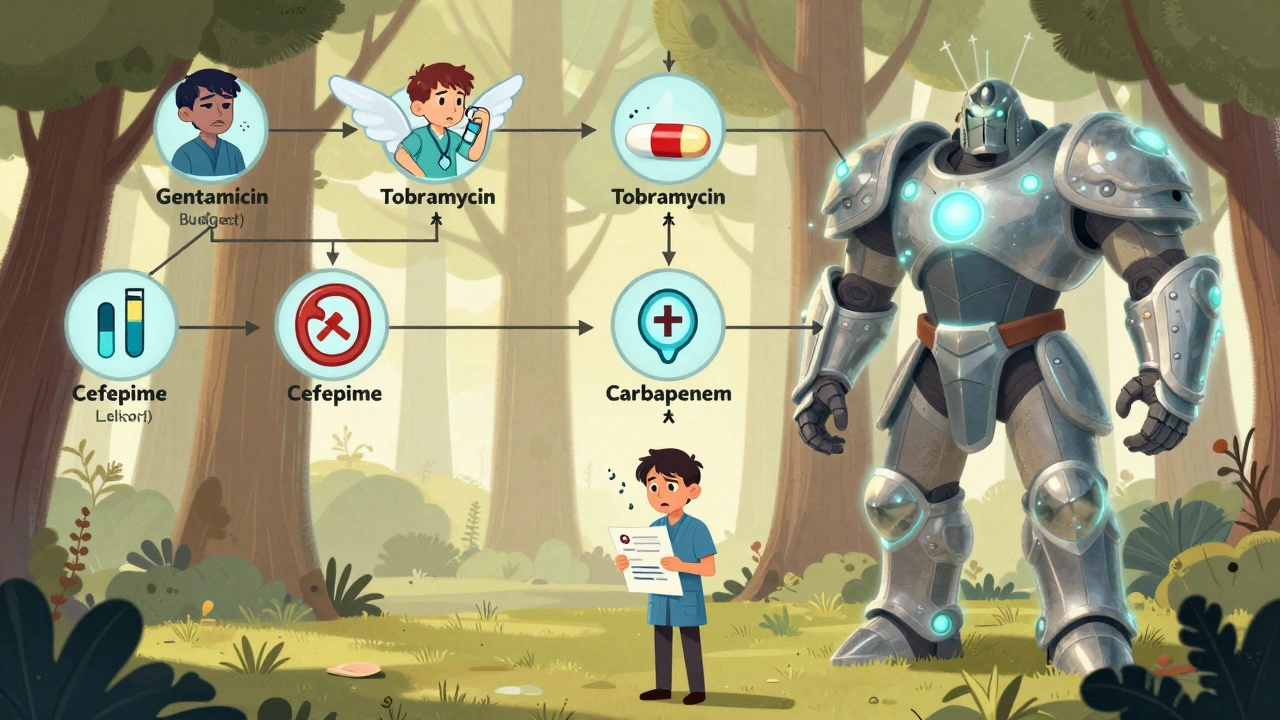
Cefepime and Other 4th-Generation Cephalosporins
Cefepime is a broad-spectrum antibiotic that belongs to the cephalosporin family, not the aminoglycosides. It’s often used as a first-line alternative to amikacin for severe infections like sepsis or complicated urinary tract infections.
Unlike amikacin, cefepime doesn’t harm hearing and has a lower risk of kidney damage. It’s also given less frequently-once every 8 to 12 hours instead of every 8 hours like amikacin.
It’s not as effective against all resistant strains, but for many common hospital infections, it’s just as good. And because it’s easier on the body, many doctors now prefer it for patients who aren’t critically ill or don’t have confirmed resistant bacteria.
Some hospitals use cefepime in combination with amikacin for very serious infections. This combo hits bacteria from two angles and reduces the chance of resistance developing.
Carbapenems: The Heavy Hitters
Meropenem and Imipenem are carbapenem antibiotics, often called the "last resort" drugs when other antibiotics fail. They’re used for multidrug-resistant infections, especially in intensive care units.
These drugs are broader than amikacin. They work against Gram-positive and Gram-negative bacteria, including some that are resistant to nearly everything. That’s why they’re reserved for the most dangerous cases.
But they’re also more expensive and can cause seizures at high doses. They’re not used unless absolutely needed. If you’ve been on multiple antibiotics already and your infection is still spreading, your doctor may switch to a carbapenem instead of increasing amikacin.
Some studies show carbapenems lead to better survival rates in sepsis caused by resistant bacteria compared to aminoglycosides like amikacin.
Fluoroquinolones: Oral Options with Caveats
Ciprofloxacin and Levofloxacin are fluoroquinolone antibiotics that come in pill form and are often used for less severe infections or as step-down therapy after IV treatment.
They’re not as strong as amikacin for life-threatening infections. But if your infection is improving and you’re stable, your doctor might switch you from IV amikacin to oral ciprofloxacin to finish the course at home.
Fluoroquinolones have their own risks: tendon rupture, nerve damage, and heart rhythm issues. The FDA has warned against using them for simple infections like sinusitis or bronchitis unless no other options exist.
They’re best used as a follow-up-not a replacement-for amikacin in serious cases.
Which Alternative Is Right for You?
There’s no single best alternative. The right choice depends on:
- What bacteria is causing the infection (confirmed by lab tests)
- Where the infection is (lung, blood, urinary tract)
- Your kidney function and hearing history
- Whether you’ve had antibiotics recently
- How sick you are
For example:
- If you have a resistant urinary tract infection and normal kidneys, cefepime might be safer than amikacin.
- If you have cystic fibrosis and a Pseudomonas flare-up, tobramycin is often the top pick.
- If you’re in the ICU with sepsis from unknown bacteria, a carbapenem may be started immediately.
- If you’re improving on amikacin and can switch to pills, ciprofloxacin might be the next step.
Doctors rarely choose antibiotics based on brand names like Mikacin. They look at the bug, the body, and the history.

Common Misconceptions
Some people think amikacin is "stronger" than everything else. That’s not true. It’s more targeted. Other drugs work better for specific bugs.
Another myth: if one antibiotic doesn’t work, you just need a stronger one. In reality, switching to a different class of antibiotic often works better than increasing the dose of the same drug.
Also, many assume that because amikacin is used in hospitals, it’s always the best. But in community settings, oral antibiotics are preferred-and often just as effective.
What to Ask Your Doctor
If you’re prescribed Mikacin Injection, here are five questions to ask:
- Why amikacin and not another antibiotic?
- Is there a less toxic option that would work just as well?
- Will I need blood tests to monitor kidney or hearing function?
- How long will I need this treatment?
- Is there an oral option to switch to later?
These questions help you understand whether amikacin is truly necessary-or if a safer, equally effective alternative exists.
Final Thoughts
Mikacin Injection (amikacin) is a powerful tool-but it’s not the only one. It’s a weapon reserved for serious, resistant infections. For many patients, gentamicin, tobramycin, cefepime, or even carbapenems may be better choices based on the infection type, patient history, and risk tolerance.
The goal isn’t to use the strongest drug. It’s to use the right drug-safely and effectively.
If you’re being treated with amikacin, don’t assume it’s the only option. Ask about alternatives. Your body will thank you.
Is Mikacin Injection the same as amikacin?
Yes. Mikacin is a brand name for the generic drug amikacin. They contain the same active ingredient and work the same way. The only differences are the manufacturer, packaging, and price. Generic amikacin is usually much cheaper and just as effective.
Can I take amikacin orally instead of by injection?
No. Amikacin is not absorbed through the digestive system, so oral tablets won’t work. It must be given as an injection or IV drip to enter the bloodstream. For less severe infections, doctors may switch you to an oral antibiotic like ciprofloxacin after you’ve improved.
How long does it take for amikacin to start working?
Most patients start to feel better within 24 to 48 hours if the bacteria are sensitive to amikacin. But you must complete the full course-even if you feel fine. Stopping early can lead to resistant infections. Doctors often check blood levels after 24 hours to make sure the dose is correct.
What are the signs of amikacin side effects?
Watch for ringing in the ears, dizziness, hearing loss, reduced urine output, swelling in the feet, or unexplained fatigue. These can signal kidney damage or nerve toxicity. Report them to your doctor immediately. Blood tests are done regularly to catch these early.
Are there any natural alternatives to amikacin?
No. There are no proven natural alternatives that can replace amikacin for serious bacterial infections. While some herbs or supplements claim antibacterial properties, none have been shown to reliably treat life-threatening infections like sepsis or pneumonia. Relying on them instead of antibiotics can be dangerous.
Can amikacin be used during pregnancy?
Amikacin is classified as Category D in pregnancy-meaning it may harm the unborn baby, especially the hearing. It’s only used if the mother’s life is at risk and no safer alternative exists. Doctors carefully weigh the risks and may monitor the baby’s development closely if it’s used.
Next Steps
If you’re currently on Mikacin Injection, keep track of your symptoms and any side effects. Ask your doctor if blood tests are scheduled. If you’re not improving after 48 hours, ask whether switching to another antibiotic might help.
If you’ve been prescribed amikacin and are unsure why, request a copy of your lab results. Knowing which bacteria you have-and whether they’re resistant to other drugs-can help you understand why amikacin was chosen.
Antibiotic decisions aren’t one-size-fits-all. The right choice depends on your body, your infection, and your history. Don’t hesitate to ask questions. Your health is worth it.



Amikacin is overused. Hospitals treat it like magic juice. Most infections don't need it. Gentamicin does the same job cheaper. Why risk kidney damage for no reason?
It is of paramount importance to recognize that the selection of an appropriate antimicrobial agent must be guided not merely by clinical intuition, but by a rigorous, evidence-based framework that integrates microbiological susceptibility profiles, pharmacokinetic-pharmacodynamic principles, and individual patient risk factors-particularly in the context of nephrotoxicity and ototoxicity, which remain significant concerns with aminoglycosides. A thoughtful, individualized approach is not merely advisable-it is ethically imperative.
Why are we even talking about alternatives? Amikacin is American-made, FDA-approved, and proven in combat. Gentamicin? That’s a third-world drug. Cefepime? Too expensive. Carbapenems? Only for the rich. Stick with what works-amikacin. We don’t need foreign substitutes when we have the best.
Amikacin? More like Ami-KABOOM. 🤯 The real question isn’t ‘which drug?’ but ‘which existential crisis are you willing to endure?’
The ontological weight of antibiotic selection transcends mere pharmacology-it’s a metaphysical negotiation between human frailty and microbial evolution. Amikacin, while potent, is but a temporal bulwark against the inevitable rise of resistance. We are not curing infections-we are merely delaying the entropy of medical certainty.
They’re hiding the truth. Amikacin causes deafness on purpose. The pharmaceutical lobby owns the FDA. They want you dependent. Watch your hearing. They’re watching you.
amikacin? bro its just a fancy word for poison. why not use garlic and turmeric? my uncle in delhi cured his pneumonia with chili paste and yoga. they dont want you to know this. big pharma is evil. 🤡
Man, this post is super helpful. I’m from Nigeria and we don’t always have access to these drugs. But knowing the alternatives helps. If gentamicin is cheaper and works, let’s use it. We need to talk more about this where I’m from.
Amikacin? More like Ami-KABOOM in the ears. 😏 Meanwhile, in India, we just use cipro and pray. No blood tests. No fancy hospitals. Just vibes and paracetamol.
Let’s be real: antibiotics aren’t about dominance-they’re about stewardship. Amikacin is a scalpel, not a sledgehammer. But too many clinicians treat it like a hammer because they’re afraid of thinking. We need humility in medicine, not bravado. If you’re prescribing amikacin without culture results, you’re not a doctor-you’re a gambler.
bro i just got off amikacin last week. 10 days of iv, 3 blood draws a day, and my ears still ring. but hey, i’m alive. thanks for the breakdown tho. cefepime sounds way better next time.
Thank you for this. I’m a nurse in Chicago, and I see so many patients terrified of amikacin because they don’t understand why it’s being used. This breakdown helps me explain it better-especially the part about switching to oral cipro after stabilization. I’m sharing this with my team.
Of course amikacin is overused. The real villain? The hospital admin who won’t pay for a culture. They’d rather burn through amikacin than wait 48 hours. And you wonder why superbugs are winning.