Stop Overpaying for Prescriptions: A Simple Way to Cut Your Medication Costs
You’re paying $45 for a 30-day supply of your blood pressure pill. Your friend pays $15 for the same pill - but they get a 90-day supply. How? They’re not cheating. They’re just using both mail-order and local pharmacies the right way.
Most people stick with one pharmacy. They go to the same local drugstore every time, even when it’s more expensive. Or they sign up for mail-order and forget they can still use their local pharmacy for emergencies. That’s leaving money on the table. The truth? You can save 20-30% on maintenance meds just by switching how you refill them.
Here’s how it works: mail-order pharmacies give you a 90-day supply at a lower cost. Local pharmacies give you immediate access. Used together, they cut your spending without sacrificing convenience or safety. You don’t need to be a healthcare expert. You just need to know which meds go where - and when.
Know Which Medications Belong in Each Place
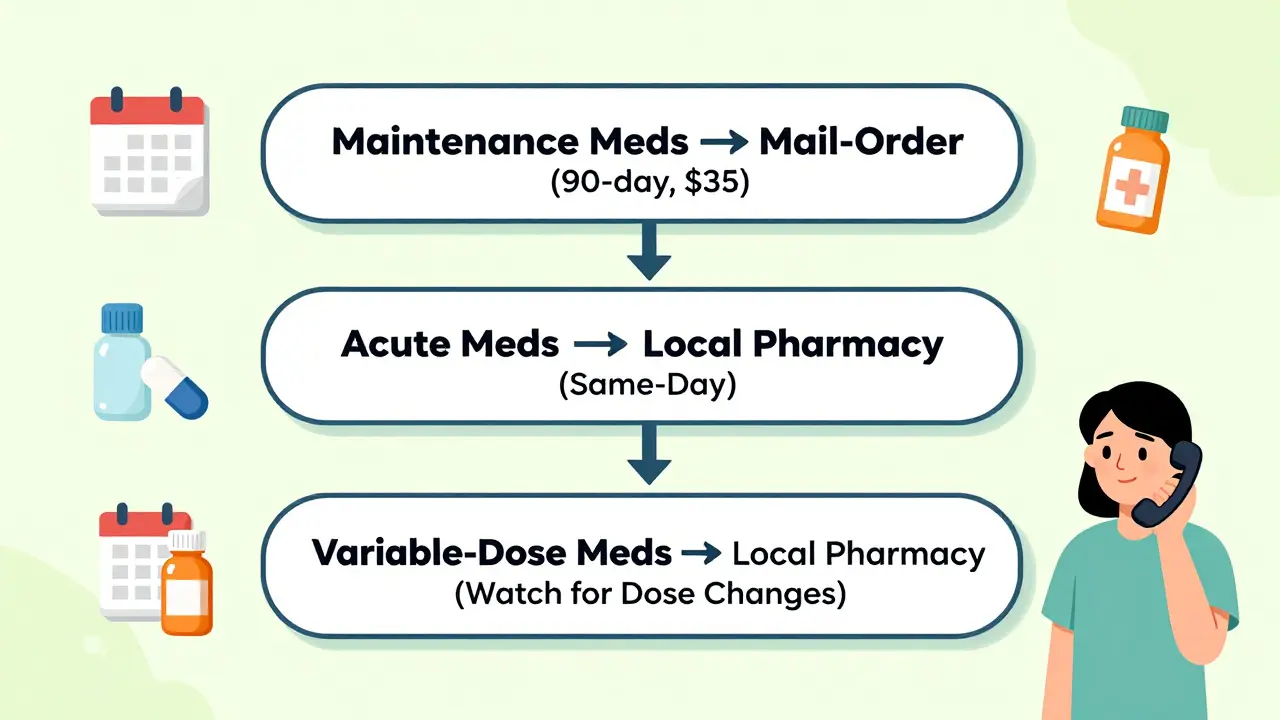
Not all prescriptions are the same. Some need steady, long-term use. Others are for emergencies or short-term fixes. The key is sorting them into three buckets.
Maintenance meds - These are the ones you take every day, for months or years. Think blood pressure pills, cholesterol drugs, thyroid medicine, diabetes meds, or antidepressants. These are perfect for mail-order. You don’t need them right now - you need them every day for the next three months. Mail-order gives you a 90-day supply at a lower copay. For example, a generic lisinopril 10mg might cost $15 for 30 days at your local pharmacy, but only $35 for 90 days through mail-order. That’s less than $0.40 per day instead of $0.50.
Acute meds - These are for sudden needs: antibiotics, painkillers after surgery, inhalers for asthma attacks, or antihistamines for allergies. These don’t work with mail-order. You can’t wait 10 days for an antibiotic when you’re sick today. Keep these at your local pharmacy. Same-day pickup saves time - and possibly your health.
Variable-dose meds - These are the tricky ones. If your doctor changes your dose often - like thyroid meds, blood thinners, or some psychiatric drugs - stick with local pharmacy. Why? Because if your dose changes, the mail-order system might still send you the old version. One Reddit user got the wrong antidepressant dose for two months because their EHR didn’t sync. They wasted $65 in pills they couldn’t use. Local pharmacists can catch those errors fast.
Mail-Order Isn’t Always Cheaper - Check Your Plan First
Many people assume mail-order is automatically cheaper. It’s not. It depends on your insurance.
Insurance plans put drugs into tiers: Tier 1 (generic), Tier 2 (preferred brand), Tier 3 (non-preferred brand), and sometimes Tier 4 (specialty). Your copay changes based on the tier - and whether you get 30 or 90 days.
For example, a Medicare Part D plan might charge:
- $45 for a 30-day Tier 3 brand-name drug at a local pharmacy
- $115 for a 90-day supply through mail-order
That’s a 24% savings per day. Great. But another plan might charge $120 for the same 90-day mail-order supply - making it more expensive than three separate 30-day fills.
Don’t guess. Call your insurer. Ask: “What’s my copay for a 90-day supply of [medication name] through mail-order versus a 30-day supply at a retail pharmacy?” Write it down. Do this for every maintenance med.
And here’s a secret most people miss: many local pharmacies offer 90-day fills at mail-order prices. CVS, Walmart, and Rite Aid all let you get 90-day generic prescriptions for the same price as mail-order - if you ask. Walmart’s $10 generic program covers 90-day supplies for some meds. No shipping. No waiting. Just walk in.
Set Up a System - Don’t Rely on Memory
Once you know which meds go where, you need a system. Otherwise, you’ll run out. And running out means emergency trips - or worse, skipping doses.
Here’s how to build a simple refill schedule:
- Make a list of all your meds. Mark each as maintenance, acute, or variable-dose.
- Check how long each maintenance med lasts. Most 90-day supplies last 90 days - but if you take one pill a day, you’re good. If you take two, it lasts 45 days.
- Set calendar reminders 10-14 days before each mail-order med runs out. Why 10-14 days? Mail-order takes 7-14 days to arrive. If you wait until you’re out, you’ll be without meds.
- Use a pill organizer for your local pharmacy meds. It’s easier to track.
One user on Reddit saved $427 a year by switching their amlodipine to mail-order and setting a calendar reminder. They said: “I used to forget until I was out. Now I get it before I run out. No stress.”
Apps like Medisafe or MyTherapy can help automate this. Or just use your phone’s built-in calendar. The point isn’t the tool - it’s the habit.
Build a Relationship With Your Local Pharmacist
Mail-order is efficient. But it’s impersonal. You can’t walk in and ask, “Is this new pill safe with my other meds?” Your local pharmacist can.
Pharmacists are trained to spot drug interactions, side effects, and dosing issues. A 2011 study found 78% of patients felt more confident with face-to-face advice than phone calls from mail-order services.
Even if you use mail-order for most meds, pick one local pharmacy you trust. Go in every few months - even if you don’t need a refill. Ask: “Can you review all my meds? Any savings I’m missing?”
Many pharmacists will run a free medication therapy review. They’ll check for duplicates, outdated prescriptions, or cheaper alternatives. The American Pharmacists Association says 40% of patients could save $200+ a year just by doing this once a year.
Watch Out for These Three Pitfalls
It’s not all easy. Here are the three most common mistakes - and how to avoid them.
1. Assuming mail-order is always cheaper - As we saw, some plans charge more. Always compare.
2. Forgetting to update your mail-order when your dose changes - If your doctor increases your dose, mail-order won’t know unless you call. Always notify them. Keep a note in your phone: “Call mail-order after every doctor visit.”
3. Not checking for local pharmacy discounts - CVS’s $4/$10/$25 program, Walmart’s $10 generics, and GoodRx coupons can beat mail-order prices. Use them. Even if you use mail-order for most things, use these for your acute meds or new prescriptions.

What’s Changing in 2026 - And What It Means for You
Things are shifting. In 2024, Medicare Part D started standardizing 90-day copays across mail-order and retail. That means the old advantage of mail-order might shrink. But here’s the good news: insurance companies are starting to integrate systems.
UnitedHealthcare’s Optum Perks now lets you switch between mail-order and local pharmacy with one click. Express Scripts lets you sync refill schedules. Epic’s new Pharmacy Navigator tool - launched in late 2023 - automatically recommends the cheapest, fastest option based on your meds and plan.
By 2026, most plans will have these tools. But until then, you’re still in control. You don’t need to wait for tech to fix this. You can start saving today.
Start Today: Your 5-Minute Action Plan
You don’t need to overhaul your life. Just do this:
- Grab your medication list. Circle the ones you take daily for months.
- Call your insurance. Ask for the copay for 30-day and 90-day supplies of each.
- Check Walmart, CVS, and GoodRx for local 90-day prices.
- Set a calendar reminder 10 days before your next mail-order refill.
- Visit your local pharmacy this week. Ask for a free med review.
That’s it. In five minutes, you’ve started saving. Most people never do. You’re already ahead.
Can I use mail-order for all my prescriptions?
No - and you shouldn’t. Mail-order is best for long-term, stable medications like blood pressure or cholesterol pills. Avoid it for new prescriptions, antibiotics, or meds that need frequent dose changes. Those should come from your local pharmacy, where you can get them immediately and talk to a pharmacist if something feels off.
Why is my mail-order refill taking so long?
Most mail-order pharmacies take 7-14 business days to deliver. That’s because they ship from a central warehouse, not your neighborhood store. If you need the med within 24-48 hours, don’t wait - go to your local pharmacy. Always order refills 10-14 days before you run out to avoid gaps.
Does my insurance even offer mail-order?
Most commercial plans and Medicare Part D do - but not all. Check your plan documents or call your insurer. Even if mail-order is offered, your copay might be higher than retail for certain drugs. Always compare prices before switching.
Can I get 90-day supplies at my local pharmacy?
Yes - and you should ask. Many pharmacies like Walmart, CVS, and Rite Aid offer 90-day fills at the same price as mail-order. You just have to request it. Ask: “Do you offer 90-day generic fills at the same price as mail-order?” Most say yes.
I’m on Medicare. Should I use mail-order?
For maintenance meds, yes - but check your specific plan. Medicare Part D plans vary. Some have lower copays for mail-order, others don’t. Use the Medicare Plan Finder tool to compare prices for your exact meds. You might find your local pharmacy already offers the same price without shipping delays.
What if I run out of a mail-order med before it arrives?
Go to your local pharmacy. Most insurers allow a one-time emergency 30-day fill if you’re out of meds. Call your plan first to confirm coverage. Keep a small backup supply of critical meds (like insulin or heart pills) if you’re prone to delays.
How often should I review my medication plan?
At least once a year - or anytime your doctor changes a prescription. Insurance plans change yearly. Your meds might change. A drug you used to pay $15 for might now be $40. A new generic might have dropped in price. A pharmacist can help you spot these shifts and save money.
Next Steps: What to Do After You Start Saving
Once you’ve got your system going, keep it simple. Review your prescriptions every six months. Look at your last three pharmacy bills. Are you still getting the best price? Did your insurer change their formulary? Did a new generic come out?
If you’re on a fixed income, look into patient assistance programs. Many drugmakers offer free or low-cost meds to those who qualify. Your pharmacist can help you apply.
And remember - saving on meds isn’t about being frugal. It’s about being smart. You’re not skipping care. You’re making sure you can afford it for years to come.



This whole post is just a glorified ad for mail-order pharmacies. I've been using them for years and the delays are insane. Got my blood pressure med late last winter and nearly ended up in the ER. Save yourself the headache and just go local.
The real issue here isn't mail-order versus local-it's the structural absurdity of pharmaceutical pricing in the first place. We've turned healthcare into a commodity game where the only winners are the middlemen and the shareholders. The fact that you need a spreadsheet and a PhD in insurance jargon just to afford lisinopril speaks volumes. This isn't smart living-it's surviving a broken system.