When a teenager stops eating, withdraws from friends, or starts failing classes out of nowhere, it’s easy to blame hormones or teenage rebellion. But when sadness lasts more than two weeks, doesn’t lift with time, and comes with sleep loss, fatigue, or talk of not wanting to live - that’s not just moodiness. That’s depression. And for kids and teens, it’s one of the most urgent mental health issues today.
In New Zealand, where I live, one in five adolescents reports feeling depressed most days. Globally, the numbers are even starker. The child and adolescent depression crisis isn’t going away. It’s growing. And the way we treat it needs to change - fast.
What Does Depression Look Like in Kids and Teens?
Depression in children doesn’t always look like crying or saying, “I’m sad.” A 10-year-old might throw tantrums, refuse to go to school, or complain of stomachaches every morning. A 15-year-old might spend hours on their phone, stop hanging out with friends, or suddenly get angry over small things. They might say, “I’m fine,” while their grades drop, their sleep shifts, or they start talking about feeling worthless.
The DSM-5 criteria for major depressive disorder in this age group include at least five symptoms over two weeks: depressed mood, loss of interest, weight changes, sleep problems, fatigue, feelings of guilt, trouble concentrating, or thoughts of death. Dysthymia - a chronic low mood lasting a year or more - is also common. And it’s not rare. About 13% of U.S. teens have had at least one major depressive episode.
What makes it worse? Many families don’t recognize the signs. Teachers miss them. Pediatricians sometimes chalk it up to “growing pains.” But untreated depression in youth leads to higher risks of substance abuse, academic failure, self-harm, and suicide. The 988 Suicide & Crisis Lifeline handled over 4 million contacts in 2023 - up 21% from the year before. That’s not just numbers. Those are kids screaming for help.
Medications: The FDA-Approved Options
When depression is moderate to severe, medication is often part of the solution. But not all antidepressants are safe for kids. In 2004, the FDA issued a black box warning after studies showed SSRIs could increase suicidal thoughts in some adolescents during the first few weeks of treatment. That didn’t mean SSRIs were dangerous - it meant we had to be smarter about how we use them.
Today, only two SSRIs are FDA-approved for treating depression in children and teens: fluoxetine (Prozac) and escitalopram (Lexapro). Others, like sertraline or citalopram, are sometimes prescribed off-label - but fluoxetine and escitalopram are the only ones with strong, consistent evidence for safety and effectiveness in this age group.
Fluoxetine is usually started at 10 mg per day, then increased to 20 mg if needed. Escitalopram starts at 5-10 mg, with a max of 20 mg. Dosing is always slow and careful. The goal isn’t to “fix” the child - it’s to reduce the worst symptoms so therapy can work.
Side effects? Common ones include nausea, headaches, insomnia, and jitteriness. About 11-18% of teens in clinical trials reported these, especially in the first 2-4 weeks. That’s why doctors monitor closely. Monthly check-ins are standard. And if suicidal thoughts appear or worsen, the medication is paused - not stopped - while the team re-evaluates.
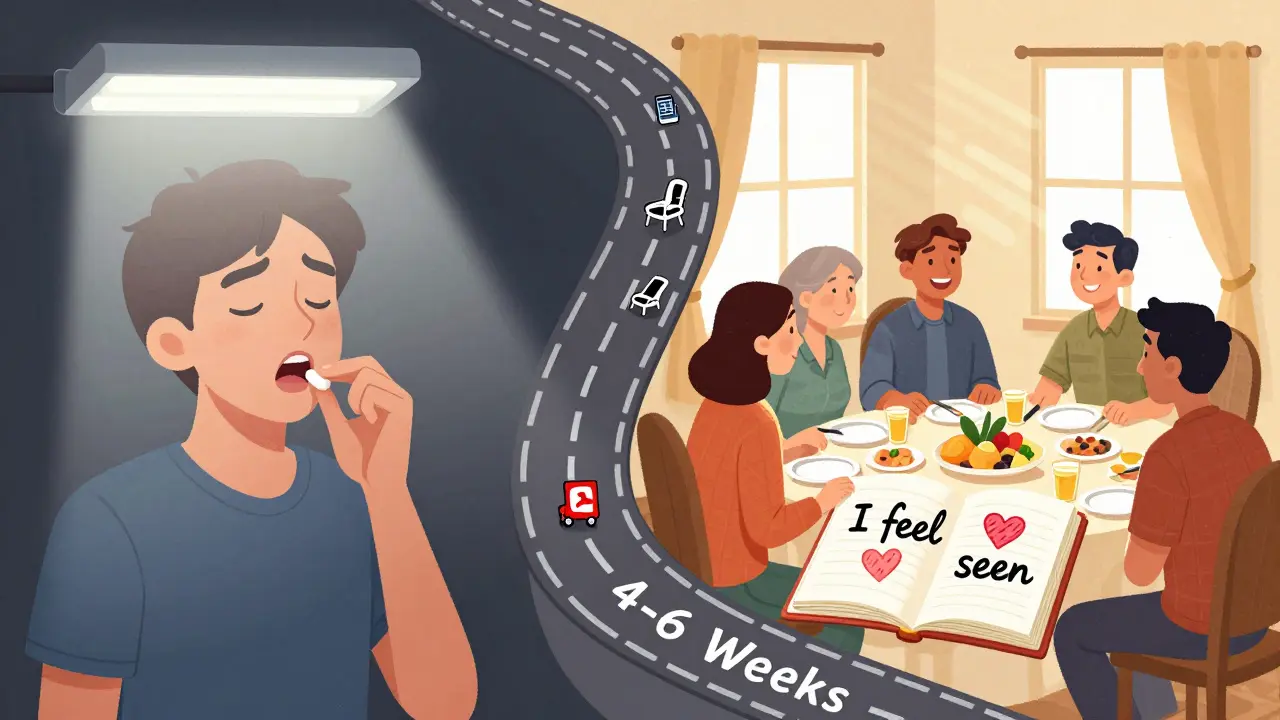
It takes 4-6 weeks for SSRIs to kick in fully. That’s hard for families to wait. But rushing to switch meds or quit early often makes things worse. Patience, paired with monitoring, saves lives.
Family Therapy: More Than Just Talking
Medication helps with symptoms. But it doesn’t fix the family dynamics that might be feeding the depression. That’s where family therapy comes in.
Not all family therapy is the same. There are different models - structural, strategic, psychodynamic, and attachment-based. But the most promising for teens with depression is Attachment-Based Family Therapy (ABFT).
ABFT isn’t about blaming parents. It’s about repairing broken emotional connections. Many depressed teens feel unheard, criticized, or disconnected from their caregivers. ABFT helps rebuild trust. One technique involves asking parents to say, “I know you’re hurting, and I want to understand - not fix - what you’re going through.” Simple. Powerful. Rarely heard in real life.
A 2022 study from Jefferson Digital Commons showed ABFT reduced suicidal thoughts in teens twice as fast as “usual care.” In just 12 weeks, 68% of teens in ABFT showed major improvement in mood and family communication. Parents reported fewer arguments, more listening, and less criticism.
But ABFT isn’t magic. It requires everyone to show up - literally and emotionally. If a parent refuses to participate, or blames the teen for everything, progress stalls. Some families walk out after session two. Others stay for 16 weeks and see their child come back to life.
Other types of family therapy focus on changing how problems are solved. Strategic therapy might ask a family to “keep the depression going” for a week - not to encourage it, but to show how the symptom keeps them stuck in old patterns. Structural therapy looks at who’s in charge: Is the teen running the house? Are parents too distant? The goal is to restore healthy hierarchy.

Family Therapy vs. Medication: Which Works Better?
There’s no single answer. But here’s what the data says:
- Medication works faster - but only for symptoms. It doesn’t teach coping skills or fix relationships.
- Family therapy works slower - but the changes last longer. Teens who complete ABFT are less likely to relapse in the next year.
- Combining both gives the best results. The Agency for Healthcare Research and Quality found that teens on SSRIs plus therapy had 40% greater improvement in daily functioning than those on therapy alone.
One 2009 NIH study followed teens in inpatient care. Those who said their family was “healthy” had a 73% recovery rate after 12 months. Those who called their family “poor” had only a 31% recovery rate - even with medication. That’s not about drugs. That’s about connection.
For teens with suicidal thoughts, ABFT is now considered a frontline treatment. For teens with severe anxiety or sleep disruption, fluoxetine might be the first step. For families with high conflict, therapy is non-negotiable.
What Families Actually Say
Real stories matter more than statistics.
On Reddit’s r/TeenDepression, a 16-year-old wrote: “My mom cried in therapy. She said she didn’t know I felt so alone. That was the first time I felt seen.” That post got over 1,200 replies. Most said the same thing: “It was hard at first. But when my parents actually listened - I got better.”
But not all experiences are positive. In NAMI forums, 41% of parents said one family member refused to attend sessions. Another 29% said the therapist took sides - either blaming the teen or the parent. That’s why choosing the right therapist matters. Look for someone trained in ABFT or structural family therapy. Ask: “Do you have experience with depressed teens? Do you work with the whole family - not just the kid?”
Parents who stuck with therapy often said the most valuable part was learning how to speak differently. Instead of saying, “Why are you so lazy?” they learned to say, “I’ve noticed you’ve been sleeping a lot. I’m worried. Can we talk?”
Barriers to Getting Help
Even with good options, access is a nightmare.
There are only 8,500 certified child and adolescent family therapists in the U.S. for 42 million teens. Waitlists in many cities are 12-18 months long. Rural areas? Often none at all.
Insurance doesn’t always cover it. Some plans only pay for 6 sessions. Others require a diagnosis before approving therapy. And many families don’t know where to start.
Telehealth is helping. New platforms like SparkTorney and Limbix offer virtual family therapy with completion rates of 72% - higher than in-person. The FDA even approved a digital therapeutic app, reSET-O, in 2023 that integrates with therapy. It’s not a replacement, but it helps families stay connected between sessions.
Cost is another issue. A single therapy session can run $150-$250. Without insurance, that’s out of reach. Some community clinics offer sliding scale fees. SAMHSA’s 2023 funding of $512 million for youth mental health includes $112 million specifically for family-based programs - but funding doesn’t always reach the people who need it most.
What You Can Do Right Now
If you suspect your child or teen is depressed:
- Don’t wait. Start with their pediatrician. Ask for a depression screening. The U.S. Preventive Services Task Force recommends universal screening for teens 12-18.
- Ask about fluoxetine or escitalopram - but only if the depression is moderate to severe. Mild cases respond better to therapy first.
- Look for a therapist trained in Attachment-Based Family Therapy (ABFT). Ask if they’re certified by the American Association for Marriage and Family Therapy.
- Join a support group. NAMI and local mental health nonprofits offer free parent workshops.
- Track symptoms. Use a simple journal: mood, sleep, school, social activity. Bring it to appointments.
- If your teen talks about suicide - call 988. Don’t wait. Don’t assume they’re “just seeking attention.”
And if you’re a teen reading this - you’re not broken. You’re not a burden. Depression is not your fault. Help exists. It’s not always easy to find - but it’s there.
The Future Is Changing
By 2030, experts predict family therapy will be a first-line treatment for nearly half of all adolescent depression cases - up from 28% today. Why? Because it works. And because it’s cheaper in the long run. Johns Hopkins estimates family therapy costs $12,500 per quality-adjusted life year - compared to $18,200 for medication alone.
Researchers are also looking at genetics. The Adolescent Brain Cognitive Development Study found certain genes may predict who responds best to SSRIs - a step toward personalized treatment.
But none of this matters if families can’t get in the door. The real breakthrough won’t be a new drug or app. It’ll be when every school, clinic, and hospital treats family therapy as a standard option - not a last resort.
Depression doesn’t live in one person. It lives in the space between people. Healing happens there too.
Can family therapy replace medication for teen depression?
For mild to moderate depression, yes - family therapy alone can be enough, especially if the family is willing to change. But for moderate to severe cases, combining therapy with fluoxetine or escitalopram gives the best results. Medication helps reduce symptoms quickly so the teen can engage in therapy. Therapy helps prevent relapse. They work best together.
Is family therapy only for teens, or can younger kids benefit too?
Yes, younger children benefit too - but the approach changes. For kids under 12, therapists often use play-based or parent-child interaction techniques. Attachment-based principles still apply: rebuilding trust, improving emotional attunement, reducing criticism. The goal is the same: help the child feel safe and understood at home.
How long does family therapy take to work?
It varies. Strategic and structural therapy often show changes in 8-10 sessions. Attachment-Based Family Therapy (ABFT) usually takes 12-16 weekly sessions. Most families report noticeable improvement in communication and mood by week 8. But lasting change takes time - and consistent participation.
What if one parent refuses to attend therapy?
It’s harder, but not impossible. Many therapists will work with the participating parent and teen first, then gradually invite the reluctant parent in. Sometimes, a single session with the resistant parent - where they’re heard without judgment - can shift the dynamic. The goal isn’t to force everyone in - it’s to create enough change in the system to help the teen heal.
Are there any risks to family therapy?
The main risk is emotional discomfort. Talking about blame, anger, or past hurts can be painful. Some families feel worse before they feel better. But trained therapists guide the process to prevent harm. The bigger risk is not doing anything at all. Untreated depression has far greater long-term consequences than temporary discomfort in therapy.
Can exercise or spirituality help with teen depression?
Yes - but not as a replacement. An eight-week online program focused on gratitude and forgiveness showed modest mood improvements in teens. Regular exercise (30 minutes, 5x/week) is as effective as medication for mild depression. Spirituality and mindfulness help some teens find meaning. But these are best used alongside therapy or medication - not instead of them.
What should I do if my teen starts having suicidal thoughts after starting medication?
Call your doctor immediately. Do not stop the medication on your own. Suicidal thoughts in the first few weeks are a known risk with SSRIs, but they’re not inevitable. Your provider may lower the dose, switch medications, or add therapy. If you’re in crisis, call 988. You’re not alone - help is available 24/7.



So fluoxetine and escitalopram are the only two FDA-approved for teens really interesting how the rest are off label but still used everywhere i wonder if that's because of insurance or just doctor habit
ABFT is just another western pseudoscience fad masquerading as therapy. In India we fix family dynamics by yelling louder and making the kid feel guilty until they snap out of it. No therapist needed. Just discipline and respect for elders.
OMG I just read this and my whole life makes sense now. My mom used to say I was just being dramatic and now I realize she was gaslighting me for YEARS. I’m 24 and still healing. THIS IS A CRISIS. WHY ISN’T THIS ON THE NEWS
Let me be clear. SSRIs don't cause suicide. The FDA black box warning was political theater. The real issue is that therapists are overworked and doctors are prescribing like candy. No one's monitoring. No one's following up. And now we're blaming the drug instead of the system.
Family therapy takes too long. Medication works faster. End of story.
So let me get this straight… we’re telling parents to say "I want to understand, not fix"… but we’re also telling teens to take antidepressants? Like… are we trying to fix the symptom or the system or just make everyone feel better for 10 minutes
Depression doesn’t live in one person. It lives in the space between people. That line… that’s the whole thesis. We treat mental illness as if it’s a broken widget inside the child. But it’s a broken rhythm in the family. The medicine just quiets the noise. The therapy rebuilds the song.
Big Pharma pushed SSRIs because they make billions. Therapy? Can’t patent it. That’s why insurance won’t cover it. The whole system is rigged. And they want you to think it’s about your kid’s brain chemistry when it’s really about profit margins
My cousin did ABFT and now she hugs her mom again 😭 I cried watching the session video. Family therapy isn’t just talk-it’s like emotional CPR. 🫂
Why is no one talking about the school system? Kids are crushed under homework and social media pressure and we act surprised they break down
If we’re measuring recovery by family communication scores, are we really treating depression or just managing family conflict? Are the two even separable?
My sister took fluoxetine for 8 months. She didn’t get better until we started family dinners again. No meds. Just sitting together. No phones. Just talking. That’s the real treatment.
As a British clinician, I find the American focus on individual pathology deeply problematic. In the NHS, we prioritize systemic intervention. Family therapy is not optional-it is standard. The U.S. system prioritizes speed over sustainability. This is not healthcare. It is triage.
India has 1 therapist per 100000 people. You think ABFT will work here? First we need schools to stop bullying kids for being smart. Then maybe therapy