Drinking alcohol with diabetes isn’t a simple yes or no question. It’s a balancing act-one that can save your life if done right, or send you to the hospital if ignored. For people with diabetes, alcohol doesn’t just affect how you feel after a night out. It directly interferes with your body’s ability to keep blood sugar stable. And the danger isn’t just during the drink-it lasts for hours after.
Why Alcohol Is Risky for People with Diabetes
Alcohol messes with your liver’s job. Normally, your liver releases glucose into your bloodstream when your blood sugar drops. But when alcohol is in your system, your liver prioritizes breaking down the alcohol instead. That means no glucose gets released. For someone on insulin or medications like sulfonylureas, this can lead to a sudden, dangerous drop in blood sugar-even if you ate before drinking. This isn’t theoretical. Research from Breakthrough T1D shows about 30% of people with type 1 diabetes who drink alcohol experience at least one severe hypoglycemic episode linked to drinking. And the symptoms? Dizziness, sweating, confusion, shakiness-sound familiar? They’re the same as being drunk. That’s why someone passing out after a few drinks might be mistaken for being intoxicated, when they’re actually having a medical emergency.What Counts as One Drink?
Not all drinks are created equal. A standard drink is defined by medical guidelines as:- 12 ounces (360 mL) of regular beer (5% alcohol)
- 5 ounces (150 mL) of wine (12% alcohol)
- 1.5 ounces (45 mL) of hard liquor like vodka, gin, or whiskey (40% alcohol)
Which Drinks Are Safest?
Your choice of drink matters more than you think. Drinks high in sugar or carbs can spike your blood sugar first, then crash it later. Here’s what to pick:- Safest options: Dry red or white wine, light beer, hard seltzers (like White Claw or Truly), and spirits mixed with soda water or diet tonic.
- Avoid: Sweet wines, liqueurs, cocktails with regular soda, juice, or syrups. A single margarita can have up to 25 grams of carbs-enough to throw your numbers off completely.
When to Avoid Alcohol Completely
Some people should not drink at all. If you have:- Diabetic neuropathy (nerve damage)
- Pancreatitis
- Advanced liver disease
- Are pregnant

How to Drink Safely: The Step-by-Step Protocol
If you choose to drink, follow these steps every single time:- Check your blood sugar before drinking. Don’t drink if it’s below 100 mg/dL or above 300 mg/dL. Target range: 100-140 mg/dL.
- Eat food with your drink. Always. Meals should include 15-30 grams of carbohydrates-like a slice of whole grain bread, a small apple, or a handful of crackers. Drinking on an empty stomach is a fast track to hypoglycemia.
- Drink slowly. Sip over the course of an hour or more. Chugging increases risk.
- Use sugar-free mixers. Soda water, diet tonic, or plain water. No regular cola, juice, or sweetened cocktails.
- Check your blood sugar every 2 hours while drinking. And again before bed.
- Carry fast-acting glucose. Keep 15 grams of glucose tablets or gel in your pocket. Don’t rely on candy-some have fat or protein that slow absorption.
- Tell someone. Let a friend or family member know you have diabetes. If you pass out, they need to know it’s not just being drunk.
- Avoid drinking after exercise. Exercise lowers blood sugar. Alcohol does too. Together, they can crash your numbers fast.
The Hidden Danger: Nighttime Hypoglycemia
One of the most dangerous times to drink is in the evening. Alcohol’s effect on your liver lasts 8-12 hours. That means your blood sugar can drop in the middle of the night-while you’re asleep. You won’t feel it. No one else might notice either. Reddit’s r/diabetes community has thousands of posts from people who woke up with dangerously low blood sugar after drinking. One user wrote: “I had two drinks with dinner. Checked my sugar at 11 p.m.-it was 120. I went to bed. Woke up at 3 a.m. at 52. My CGM screamed. I didn’t feel a thing.” That’s why checking your blood sugar before bed is non-negotiable. If it’s under 120 mg/dL, eat a small carb snack-like half a banana or a few crackers-before sleeping.Technology Can Help
New tools are making this easier. The Dexcom G7 continuous glucose monitor now includes an “Alcohol-Diabetes Safety Algorithm.” It analyzes your glucose trends and alcohol intake to warn you of rising hypoglycemia risk in real time. In clinical trials, users who used this feature saw a 37% drop in severe low blood sugar events. The ADA is also moving toward personalized thresholds. Instead of a one-size-fits-all 100 mg/dL cutoff, they’re exploring using your personal CGM data to set safer limits based on your unique response to alcohol.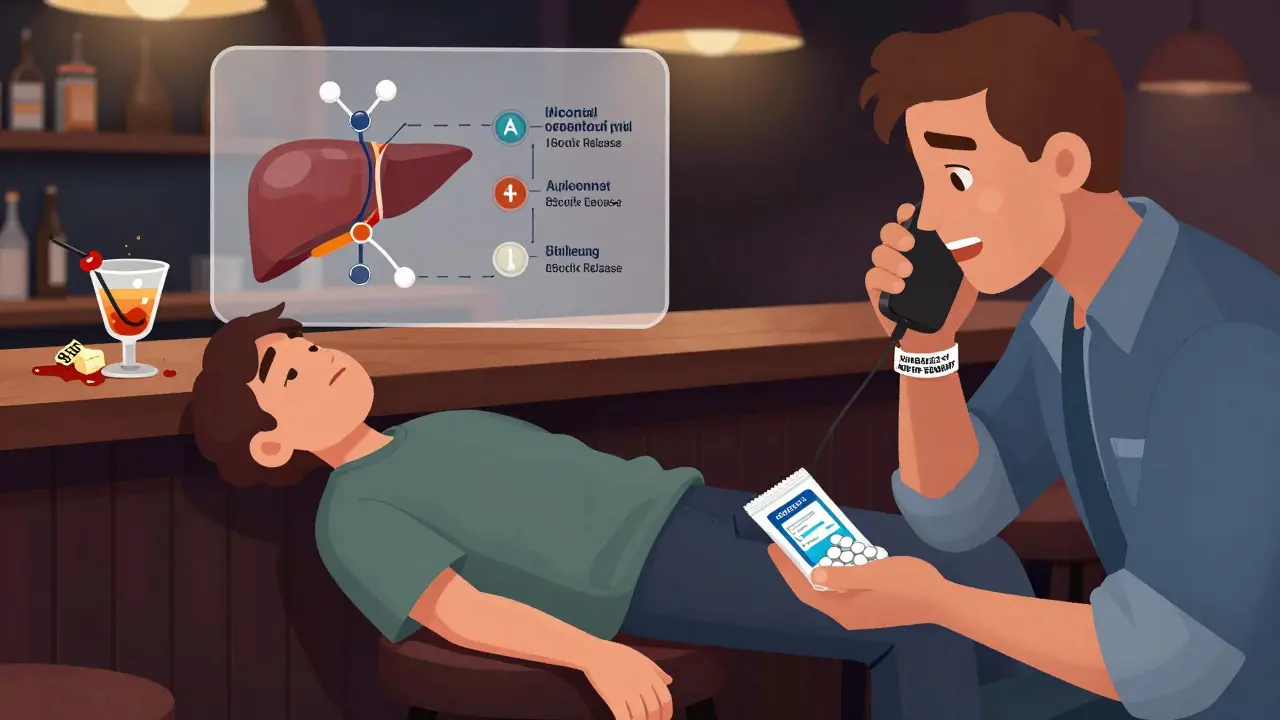
What the Research Really Says
Some studies say moderate red wine might improve insulin sensitivity by 12%. Others suggest light drinkers with type 2 diabetes have a 15-20% lower risk of heart disease. But here’s the catch: the American Diabetes Association doesn’t recommend starting to drink for these benefits. The risks outweigh the rewards for most people. And if you already drink? Stick to the rules. Don’t use “it’s good for my heart” as an excuse to skip the precautions.Real Stories, Real Risks
On Breakthrough T1D forums, 68% of users reported at least one severe low blood sugar episode after drinking. The common thread? They didn’t check their blood sugar after the drink. Or they drank without eating. Or they went to bed without a snack. The users who stayed safe? They followed the protocol. They ate. They monitored. They carried glucose. They told someone. Their hypoglycemic events dropped by 82%.Final Rule: Never Guess
Diabetes management is about control. Alcohol takes that control away. Even if you’ve drunk safely for years, your body changes. Your medications change. Your liver changes. What worked last year might not work today. The safest approach? Don’t drink. But if you do, treat it like a medical procedure. Check your numbers. Eat. Monitor. Carry rescue glucose. Tell someone. And never, ever assume you’re fine because you feel okay.What to Do If You Think You’re Having an Alcohol-Induced Low
If you or someone else is confused, shaky, sweaty, or unconscious after drinking:- Check blood sugar immediately if possible.
- Give 15 grams of fast-acting glucose-glucose tablets, gel, or juice if no tablets are available.
- If the person is unconscious or can’t swallow, call emergency services. Do NOT put anything in their mouth.
- Even if they wake up, get medical help. The risk of another drop remains for hours.
Can I drink alcohol if I have type 1 diabetes?
Yes, but with strict precautions. Alcohol increases hypoglycemia risk, especially with insulin. Always check your blood sugar before, during, and after drinking. Eat carbs with your drink. Never drink alone. Carry glucose. Monitor overnight. Many people with type 1 diabetes drink safely by following these steps.
Why does alcohol cause low blood sugar hours after drinking?
Your liver stops releasing glucose to focus on breaking down alcohol. This effect can last 8-12 hours. Even if your blood sugar was fine when you stopped drinking, your liver won’t refill it. That’s why nighttime lows are so common-and dangerous.
Is red wine safe for people with type 2 diabetes?
Dry red wine in moderation (one 5-ounce glass) is among the safest alcoholic choices because it’s low in sugar. Some studies show it may improve insulin sensitivity. But it still carries hypoglycemia risk. Always drink with food and monitor your blood sugar. Don’t start drinking just for health benefits.
Can I drink if I’m on metformin?
Moderate drinking is usually okay with metformin. But heavy drinking-more than four drinks in two hours-can raise your risk of lactic acidosis, a rare but serious condition. Stick to one or two drinks max, always with food, and avoid binge drinking.
Do I need to wear a medical alert bracelet?
Yes, especially if you drink. Emergency responders can’t tell if you’re drunk or having a low. A medical alert bracelet says “Diabetes” and “Insulin Dependent” so they can treat you correctly. Over 90% of endocrinologists recommend it for people with diabetes who drink.
What should I do if I feel fine after drinking but my blood sugar is low?
Treat it anyway. Alcohol masks the symptoms of low blood sugar. You might not feel shaky or sweaty-even if your glucose is at 60 mg/dL. Always treat a low with 15 grams of fast-acting carbs, then recheck in 15 minutes. Don’t wait for symptoms.
Are there any drinks I should avoid completely?
Yes. Sweet cocktails, liqueurs, regular sodas as mixers, and “diabetic” beers or ciders. These either spike your blood sugar first, then crash it, or have higher alcohol content that increases hypoglycemia risk. Stick to dry wine, light beer, hard seltzers, and spirits with soda water.
Can I drink after working out?
No. Exercise lowers blood sugar. Alcohol lowers it further. Together, they can cause a dangerous drop within minutes. Wait at least two hours after exercise before drinking. And always eat carbs before drinking.



I've been living with type 2 for 12 years and I still drink wine with dinner. Not every night, but sometimes. I check my sugar before, eat something with protein and fiber, and never go to bed without a quick check. It's not perfect, but it works. Just don't be lazy about it.
This is so important. I used to think I could just 'feel' when my sugar was low, until I woke up at 3 a.m. with a reading of 48 and no idea why I was sweating through my shirt. Now I always tell my partner before I drink. It's not about restriction-it's about staying alive.
The ADA’s recommended thresholds are outdated. Recent meta-analyses from the Journal of Clinical Endocrinology & Metabolism indicate that individualized glycemic response curves, derived from CGM-derived time-in-range data, demonstrate significant heterogeneity in alcohol-induced hypoglycemia kinetics. A one-size-fits-all 100 mg/dL cutoff ignores pharmacodynamic variability in insulin sensitivity postprandially and circadian hepatic glucose output suppression. You need personalized thresholds.
People act like alcohol is some kind of poison for diabetics but honestly if you're managing your meds and eating right you can handle it. The real problem is the fearmongering. I've had three drinks with pizza and my sugar was fine. Stop making us feel guilty for living
I've lived in five countries and drunk in all of them. In India, they serve lager with meals like water. In Germany, they have beer gardens where everyone checks their glucose before raising a glass. In the US, we turn it into a moral panic. The truth? Alcohol doesn't care about your nationality or your diagnosis-it only cares about your liver. If you're going to drink, treat it like you're administering insulin. Measure. Monitor. Mitigate. The cultural context matters less than the physiological reality. I've seen people in Tokyo, Toronto, and Tbilisi do this right. And I've seen people in Chicago die because they thought 'I'm fine' meant 'I'm safe'. Don't be that person.
Who told you the ADA even knows what they're talking about?? They're funded by Big Pharma and Big Alcohol!! The real reason they say 'one drink' is because they don't want you to know that alcohol is a stealthy insulin mimetic that's been used for decades to artificially lower glucose in clinical trials!! And don't get me started on Dexcom's 'Alcohol-Diabetes Safety Algorithm'-that's just a Trojan horse to get you hooked on their $1200/month monitors so they can sell you more data! They want you dependent! Wake up!! Your liver isn't 'prioritizing' alcohol-it's being poisoned by corporate greed disguised as science!!
Respectfully, the assertion that alcohol consumption may be permissible under stringent conditions, while technically accurate, remains fraught with ethical and physiological peril. The hepatic inhibition of gluconeogenesis is not merely a pharmacological inconvenience; it is a systemic vulnerability that, in the context of insulin-dependent diabetes, constitutes an existential risk. One must consider not only the individual, but the familial, societal, and economic ramifications of a hypoglycemic episode occurring in public, during transit, or while operating machinery. Therefore, while the protocol outlined is commendable, the only truly prudent course remains abstinence.
So let me get this straight... you're telling me I can't have a margarita with my tacos because some lab in Boston says my liver might 'prioritize' alcohol?? 😂 I'm not a robot. I'm a human who eats tacos, drinks tequila, and still runs 5Ks. If I check my sugar and eat a damn tortilla, I'm good. Stop making diabetes a religion.
They say 'check before bed' but what if you're at a party and you're not alone? What if your friends are drunk and you're the only one with a CGM? Who's gonna wake up to check your glucose at 2 a.m.? The system is broken. They want us to carry glucose but not tell anyone. They want us to 'tell someone' but then blame us when we're passed out and they think we're just 'wasted'. It's a trap. They don't want us to drink. They want us to be perfect. And guess what? We're not perfect. We're people. 😔
i used to drink all the time then woke up at 3am with my pump beeping like a madman and i had no idea why. now i just stick to seltzer with lime. its boring but i’m alive. no regrets.
You know what’s really scary? That Dexcom algorithm. It’s not just tracking your glucose-it’s syncing with your phone, your smartwatch, your smart fridge, your smart toilet. They’re building a profile. They know when you drink, when you eat, when you sleep. They’re mapping your body’s weakness. And then? They’ll raise your insurance rates. Or deny your claim. Or sell your data to the pharmaceutical giants who make the insulin you need. This isn’t safety. It’s surveillance. And you’re letting them do it because you’re scared of a low.