Most people think a bad cough means they need antibiotics. It’s a natural assumption-when you feel awful, you want something to fix it fast. But here’s the truth: acute bronchitis is almost never caused by bacteria. It’s a viral infection, and antibiotics won’t help. In fact, taking them when they’re not needed does more harm than good.
What Exactly Is Acute Bronchitis?
Acute bronchitis is an inflammation of the bronchial tubes-the airways that carry air to your lungs. It usually starts after a cold or flu. The main symptom? A cough. It might bring up clear, white, or yellowish mucus. You might also feel tired, have a low-grade fever, or get a sore throat. But here’s the key: it’s not pneumonia. If you don’t have a high fever, rapid breathing, or chest pain that gets worse when you breathe, you likely don’t have pneumonia.
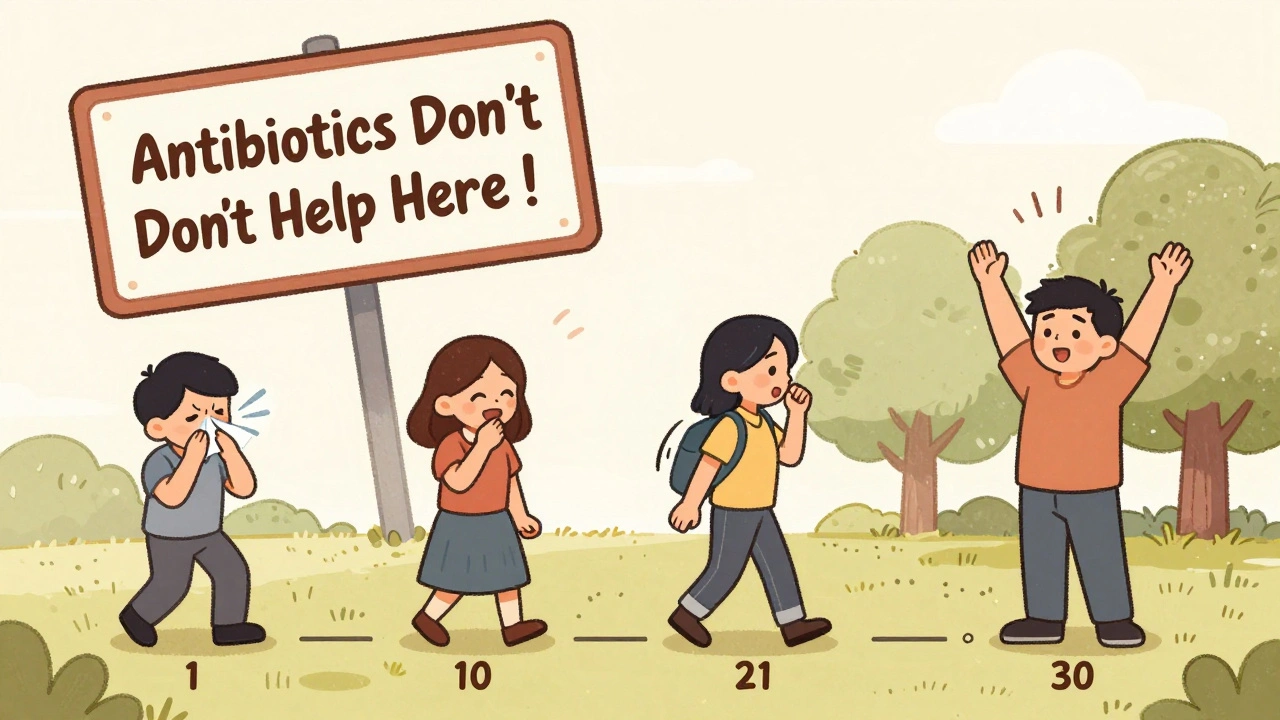
This condition is incredibly common. About 5% of adults in the U.S. get it every year. That’s roughly 10 million doctor visits annually. And despite how often it shows up, most cases clear up on their own. The cough? It lingers. Studies show half of people are still coughing after 10 days. About a quarter still have it after two weeks. And 1 in 10 are coughing at three weeks. That’s normal. It doesn’t mean you’re getting worse. It just means your airways are healing slowly.
Why Antibiotics Won’t Help (And Why They’re Dangerous)
Ninety to ninety-five percent of acute bronchitis cases are caused by viruses-rhinovirus, coronavirus, flu, or RSV. Antibiotics kill bacteria. They don’t touch viruses. So if you’re taking them for bronchitis, you’re not fighting the cause. You’re just exposing your body to side effects.
What kind of side effects? Diarrhea, nausea, rashes, yeast infections. In one study, for every 14 people given antibiotics for bronchitis, one had a bad reaction. Meanwhile, the benefit? A reduction of just 0.6 days in cough length. That’s less than half a day. Not worth the risk.
And here’s the bigger picture: every unnecessary antibiotic use contributes to antibiotic resistance. That’s when bacteria evolve to survive drugs meant to kill them. The CDC estimates 46 million unnecessary antibiotic prescriptions are given for respiratory infections like bronchitis each year in the U.S. That fuels 2.8 million resistant infections and 35,000 deaths annually. You’re not just risking your own health-you’re helping create superbugs that could one day make even simple infections deadly.
What Actually Helps: Evidence-Based Cough Care
If antibiotics won’t work, what will? The answer is simple: time, hydration, rest, and smart symptom relief.
- Drink fluids. Aim for 8-10 glasses of water a day. It thins mucus and keeps your throat moist. Warm tea or broth helps too.
- Rest. Your body needs energy to fight the virus. Pushing through work or workouts won’t speed things up.
- Use a humidifier. Cool-mist humidifiers add moisture to dry indoor air, which soothes irritated airways. Clean it daily to avoid mold.
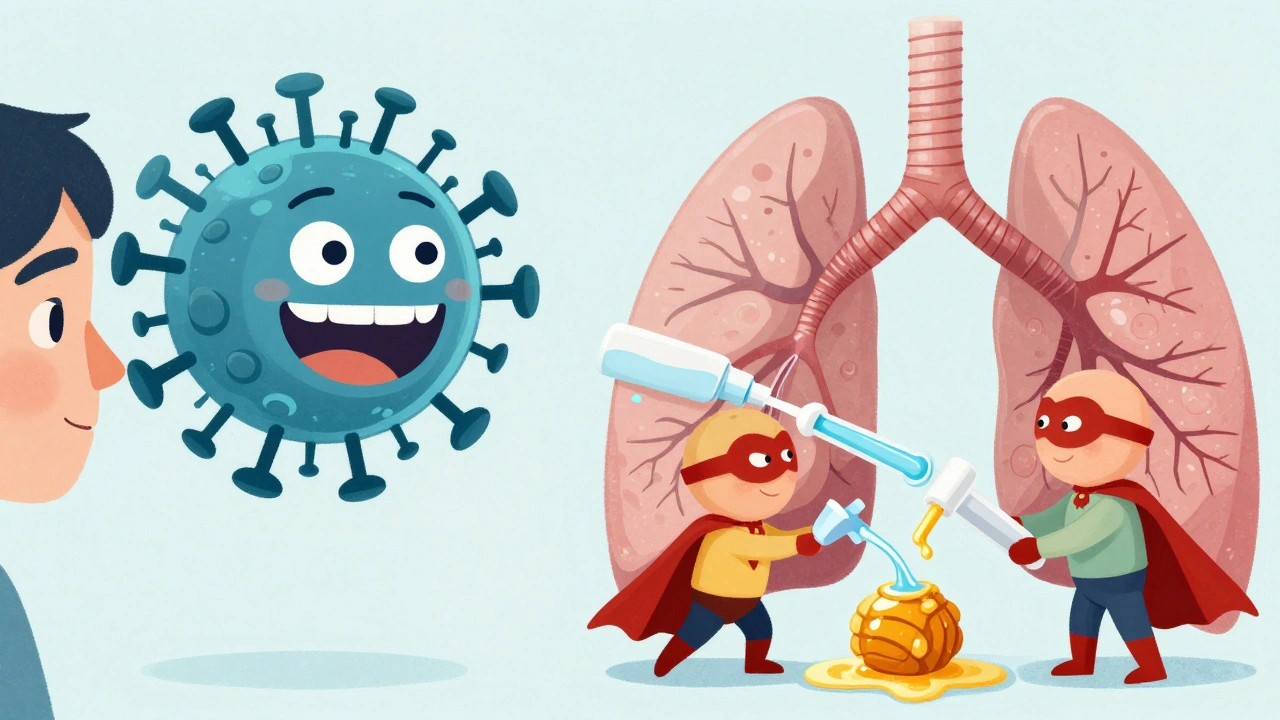
- Try honey. For adults and kids over 1 year old, 1-2 teaspoons of honey before bed can reduce nighttime coughing better than many over-the-counter syrups. One study showed it worked as well as dextromethorphan, without the side effects. Important: Never give honey to babies under 12 months-it can cause botulism.
- Use ibuprofen or acetaminophen. For body aches or fever, take them as directed. Don’t exceed 3,000 mg of acetaminophen per day if you have liver issues.
For cough suppressants, dextromethorphan (found in many OTC syrups) has modest benefit. It’s not magic, but it can help you sleep. Dose: 15-30 mg every 6-8 hours, max 120 mg per day. Avoid codeine or hydrocodone cough medicines-they’re risky, especially for kids. The FDA banned them for children under 12 in 2018.
What Doesn’t Work (And Why You Should Skip It)
Some treatments are popular but lack solid proof.
- Guaifenesin (Mucinex): This expectorant claims to loosen mucus, but studies show mixed results. Only 2 out of 7 trials found real benefit. Don’t count on it.
- Inhalers or bronchodilators (like albuterol): These help wheezing. But if you don’t wheeze, they won’t help your cough-and they can cause jitteriness, fast heartbeat, or tremors. Only use them if your doctor confirms wheezing is present.
- Antibiotics: Again, no. Not for viral bronchitis. Not even if your mucus is yellow or green. That’s normal with viral infections. Color doesn’t mean bacterial.
When to See a Doctor
You don’t need to rush to the clinic for every cough. But call your provider if:
- Your cough lasts longer than 3 weeks
- You have a fever above 38°C (100.4°F) that lasts more than a few days
- You’re wheezing, short of breath, or coughing up blood
- You have chest pain that gets worse when you breathe
- You have a weakened immune system, COPD, asthma, or heart disease
These signs could mean pneumonia, asthma flare-up, or another condition that needs different treatment. Don’t wait if you’re concerned.
How Doctors Are Changing Their Approach
For years, doctors gave antibiotics for bronchitis because patients asked for them-and because it was easier than explaining why they weren’t needed. But things are shifting.
Guidelines from the American Academy of Family Physicians, the CDC, and the American College of Chest Physicians all agree: don’t prescribe antibiotics for uncomplicated acute bronchitis. The evidence is clear. Still, in 2022, over half of bronchitis visits ended in an antibiotic prescription. Rates are higher in the South (62%) than in the West (38%).
Doctors are now using better communication tools. One study found that using a simple 5-question survey to check patient expectations cut antibiotic requests by 32%. Another approach? Give a delayed prescription. You leave the office with a script for antibiotics-but you’re told to fill it only if you’re worse after 48-72 hours. Most people never do.
Future research is looking at natural options like ivy leaf extract. Early results are promising, but nothing beats the basics: rest, fluids, and patience.
The Bottom Line
Acute bronchitis is annoying. It can last weeks. But it’s not dangerous for most healthy people. Antibiotics won’t cure it. They won’t shorten it meaningfully. And they might make things worse-for you, and for everyone else.
Focus on what actually helps: sleep, water, honey, and time. Your body is built to heal itself. Trust it. And if a doctor pushes antibiotics, ask: ‘Is this really necessary?’ You’re not being difficult. You’re being smart.
Are antibiotics ever used for acute bronchitis?
Antibiotics are rarely used for acute bronchitis. They’re only considered if there’s strong evidence of a bacterial infection-like whooping cough (pertussis) or in people with chronic lung diseases such as COPD. For healthy adults with a typical viral cough, antibiotics provide no meaningful benefit and carry risks. The CDC and major medical groups strongly advise against them.
Why does my cough last so long?
The virus that causes bronchitis damages the lining of your airways. Even after the infection clears, the nerves in your bronchial tubes stay extra sensitive. This makes you cough at the slightest irritation-like cold air, smoke, or even talking. It’s not an ongoing infection. It’s your body’s healing response. Most coughs fade between 2 and 3 weeks, but 1 in 10 people still cough at 3 weeks. That’s normal.
Is green or yellow mucus a sign I need antibiotics?
No. Colored mucus-green, yellow, or even brown-is common with viral infections. It’s caused by white blood cells fighting the virus, not by bacteria. Many people think colored mucus means infection, but studies show it’s not a reliable indicator. Doctors rely on symptoms like fever, breathing trouble, or chest pain-not mucus color-to decide if antibiotics are needed.
Can I give honey to my child for cough?
Yes-for children over 1 year old. Honey has been shown to reduce nighttime coughing better than many OTC cough syrups. Give 1 to 2 teaspoons before bed. But never give honey to babies under 12 months. It can cause infant botulism, a rare but serious illness. For babies under 1, use a humidifier and saline drops instead.
What’s the best way to prevent acute bronchitis?
The best prevention is avoiding viruses. Wash your hands often, avoid touching your face, and stay away from people who are sick. Get your yearly flu shot-it reduces your risk of catching flu, which often leads to bronchitis. If you smoke, quitting is the single most effective way to protect your lungs. Smoking damages the airway’s natural defenses, making you much more likely to get bronchitis-and more likely to have it recur.



So let me get this straight-we’ve got millions of people getting antibiotics for a virus because they think green snot = bacterial invasion? And we wonder why superbugs are winning? 🤦♂️
Let’s be clear: the fact that 50%+ of physicians still prescribe antibiotics for viral bronchitis is a catastrophic failure of medical education, public health literacy, and institutional inertia. The data is unambiguous-antibiotics offer negligible benefit, significant risk, and contribute to a global health crisis. This isn’t ‘alternative medicine’-it’s evidence-based medicine being ignored by a system that prioritizes convenience over competence.
And don’t get me started on the ‘honey works’ crowd-yes, it’s marginally better than dextromethorphan in one RCT, but let’s not turn Grandma’s kitchen cabinet into a clinical guideline. We need systemic change, not folk remedies.
Meanwhile, the CDC’s 46 million unnecessary prescriptions per year? That’s not a statistic-it’s a public health crime.
Hi everyone. I’m a nurse in rural Ohio, and I see this every single week. People come in with coughs lasting three weeks, convinced they need antibiotics. I hand them the pamphlet, explain the virus timeline, and suggest honey and fluids. Most leave skeptical. But I’ve had a few come back two weeks later saying, ‘You were right-I didn’t need anything but rest.’ It’s small victories, but they matter.
Also, never underestimate the power of a warm tea and a listening ear. Sometimes that’s the real medicine.
yo i was sick last month and doc gave me amoxi and i felt better but now i read this and i think maybe it was just time?? also honey is legit good i put 2 tsp in tea and slept like a baby 🤓
There’s something deeply ironic about how we treat acute bronchitis: we’re willing to wait out a cold for seven days, but when the cough lingers past ten, we panic and demand a chemical solution. The human body is not a machine that needs a reset button. It’s a self-correcting system that requires patience, not pharmaceutical intervention.
The real tragedy isn’t the cough-it’s the erosion of trust in our own biology because we’ve been conditioned to believe that discomfort must be immediately erased.
In the UK, we call this ‘the winter cough’-it’s practically a rite of passage. My grandmother used to say, ‘Let it run its course, love.’ She never took antibiotics for anything, lived to 94, and never had a hospital stay. There’s wisdom in letting nature take its time.
And honey? Yes. Always honey. Even my Scottish uncle, who thinks tea should be strong enough to strip paint, swears by it.
Y’ALL. I had bronchitis last winter and I was SO ready to beg for antibiotics. But I read this exact article and thought-wait, maybe I don’t need them. I drank water like it was my job, slept 10 hours a night, and put honey on my toast before bed. Cough lasted 18 days. Felt like forever. But I didn’t get sick again for months. And I didn’t ruin my gut flora. WINNING.
Also-humidifier = magic. Buy one. You’ll thank me.
Antibiotics don't work. Cough lasts weeks. Honey helps. Don't take them.
I can’t believe we’re still having this conversation in 2025. I’m a pharmacist, and I’ve watched patients cry because their doctor refused to give them antibiotics. They think it means I’m not listening. But I’m listening SO hard-I’m listening to the science, to the CDC, to the fact that every unnecessary pill is another step toward a world where penicillin doesn’t work anymore.
And honey? I literally keep a jar on my counter for my own kids. I’ve even started handing out little sample packets at the counter. It’s not a cure-it’s a kindness.
i just wanted to say i got the cough too and i didnt take anything and it went away. also i dont trust doctors anymore. they just want to sell stuff.
My mom used to say, ‘Your body’s got a mind of its own.’ I didn’t get it until I was 32 and spent three weeks coughing my lungs out after a cold. No meds. Just tea, steam, and naps. I felt like a zombie, but I didn’t take a single antibiotic. And guess what? I didn’t get sick again all winter.
It’s not about being tough. It’s about trusting what your body already knows how to do. We’ve been trained to fear discomfort-but sometimes, discomfort is just healing in disguise.
Also, honey on toast before bed? That’s my new bedtime ritual. It’s not magic. But it feels like love.
Let’s be honest: the entire ‘honey works’ narrative is a bourgeois fantasy peddled by wellness influencers who’ve never worked a 12-hour shift in a factory or raised a kid on minimum wage. Most people don’t have the luxury of ‘resting’ for three weeks. They need a quick fix-whether it’s antibiotics or a placebo. And if antibiotics give them psychological relief? Fine. Let them have it. The real problem isn’t antibiotic resistance-it’s the structural inequities that make people desperate for any solution, however flawed.
Also, RSV? That’s a real threat. But you won’t hear Big Pharma talking about that. They’d rather sell you a $20 bottle of honey.
bro i just used a humidifier and it was like a whole new person 😌 i was coughing so bad i woke up crying and now i’m fine. also honey is the GOAT 🍯
10/10 post. 🙌 I’ve been telling my coworkers for years that green mucus doesn’t mean antibiotics. They still don’t believe me. I’m just gonna keep sending them this link. Maybe one day we’ll stop treating our bodies like broken phones.
There is a deeper philosophical question here: Why do we equate intervention with care? Why do we believe that suffering must be eradicated rather than understood? The cough is not an enemy-it is a messenger. It is the body’s language, its protest, its slow, stubborn insistence on healing. To silence it with chemicals is not to heal-it is to suppress. We have become a civilization terrified of silence, terrified of stillness, terrified of the natural rhythm of recovery. We reach for pills because we cannot bear the weight of waiting. But perhaps the most radical act of medicine today is not prescribing-but pausing.
Jim, you’re right about the systemic failure-but you’re also ignoring the human side. People aren’t dumb. They’re scared. They’ve been told for decades that ‘if you’re sick, there’s a pill for it.’ You can’t fix that with data alone. You need empathy. You need doctors who say, ‘I get it. This sucks. But here’s what’s actually going on.’
That’s why I love the delayed prescription trick. It gives the patient control. It validates their fear. And it still stops 90% of antibiotics from being used.