Most kids get colds. It’s normal. A preschooler might have 8 to 12 ear infections, runny noses, or coughs in a year. But when those infections don’t stop - when they get worse, don’t respond to antibiotics, or show up in strange places - it’s not just bad luck. It could be a sign something’s wrong with the immune system.
When Is a Recurrent Infection a Red Flag?
Not every infection means immunodeficiency. But certain patterns should make you pause. The American Academy of Allergy, Asthma & Immunology and the European Society for Immunodeficiencies agree on key warning signs. If a child or adult has:
- Four or more ear infections in one year
- Two or more serious sinus infections in 12 months
- Two or more pneumonias within a year
- Deep skin or organ abscesses that keep coming back
- Oral thrush (white patches in the mouth) after age one
- Infections that need IV antibiotics to clear
- Infections caused by unusual organisms like Pneumocystis jirovecii or fungal infections in healthy tissue
- Failure to gain weight or grow normally
- A family history of early deaths from infection or known immunodeficiency
These aren’t just "bad luck." They’re signals. A child with recurrent pneumonia and no response to two full courses of antibiotics isn’t just sensitive to germs - their body may not be able to fight them at all. An adult with chronic fungal skin infections and no diabetes or steroid use? That’s not eczema. That’s a red flag.
What Does a Normal Immune System Look Like?
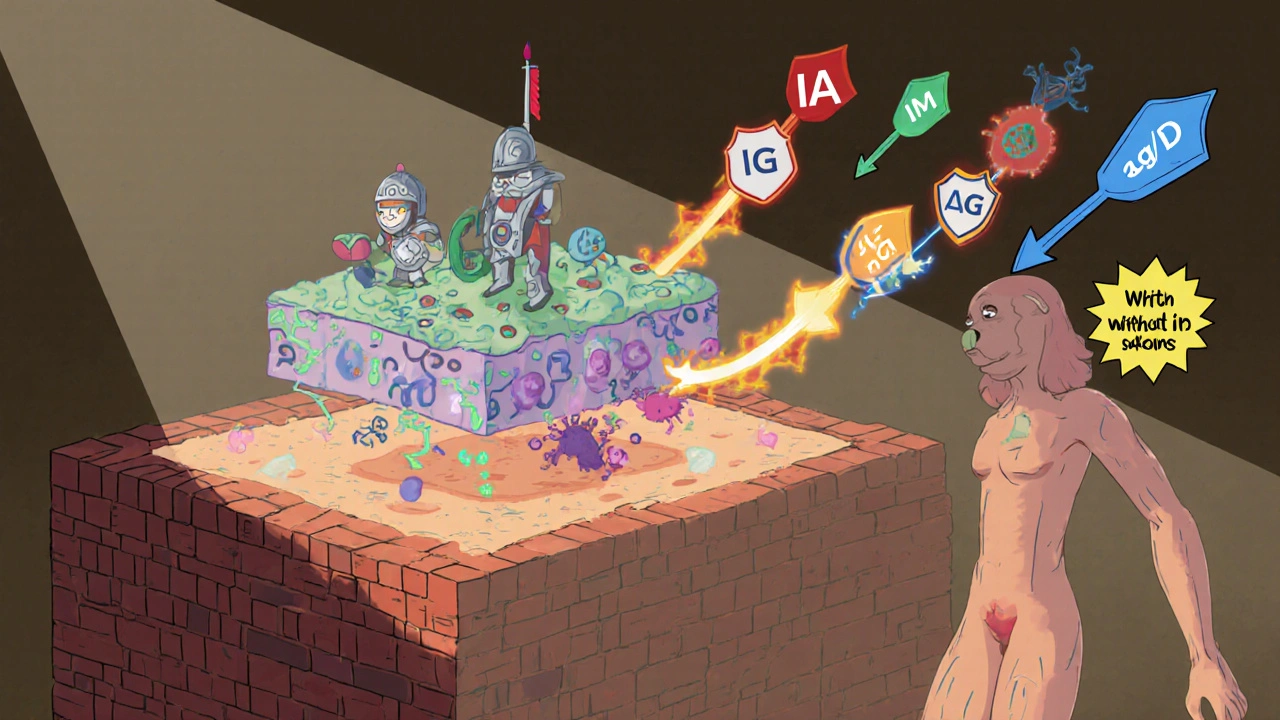
To spot when something’s broken, you need to know what’s working. A healthy immune system has three layers: physical barriers (skin, mucus), innate defenses (white blood cells that attack anything strange), and adaptive immunity (antibodies and T-cells that learn and remember specific threats). Antibodies - IgG, IgA, IgM - are the body’s targeted weapons. They’re made by B-cells and circulate in the blood to neutralize bacteria and viruses.
But antibody levels change with age. A 3-month-old baby can have an IgG level of 243 mg/dL and be perfectly normal. By age 5, that same child should be near adult levels - 700 to 1,600 mg/dL. If a 7-year-old has an IgG of 420 mg/dL, that’s not "just low." It’s dangerously low for their age. Many doctors miss this because they compare it to adult ranges. That’s a common mistake.
How Do You Test for Immunodeficiency?
Testing isn’t one blood draw. It’s a step-by-step process.
Step 1: Complete Blood Count (CBC) with Differential
This checks your white blood cell count. In kids over one year, lymphocytes below 1,500 cells/μL raise concern. In infants under one, below 3,000 is a red flag. Low lymphocytes mean fewer soldiers in the immune army.
Step 2: Immunoglobulin Levels
Measure IgG, IgA, and IgM. But you must use age-adjusted ranges. IgA is often the first to drop in common variable immunodeficiency (CVID). If IgG is below 400 mg/dL and IgA and/or IgM are also low, that’s a strong indicator of CVID - especially if the patient can’t make antibodies after vaccines.
Step 3: Vaccine Response Test
This is the gold standard. Give a tetanus or diphtheria shot, wait 4 to 6 weeks, then check antibody levels. Protective levels? At least 0.1 IU/mL for tetanus. For pneumococcal vaccine (the polysaccharide kind), you need at least 1.3 μg/mL for each serotype. If the body doesn’t respond, the immune system isn’t learning - and that’s a problem.
Step 4: Flow Cytometry
This test counts T-cells (CD3, CD4, CD8) and B-cells (CD19). In severe combined immunodeficiency (SCID), CD3+ T-cells can be below 1,000 cells/μL in a 2-year-old. In X-linked agammaglobulinemia, B-cells are nearly absent. This test can show if the problem is in the cells themselves, not just the antibodies they make.
Don’t skip the vaccine challenge. A patient with IgG at 450 mg/dL might seem okay - until you find they can’t make a single protective antibody after a vaccine. That’s CVID. And it needs treatment.
What Else Could Be Causing Recurrent Infections?
Before jumping to immunodeficiency, rule out the obvious. Up to 43% of kids with frequent infections have anatomical problems - not immune ones. Cystic fibrosis causes thick mucus that traps bacteria. Chronic sinusitis from deviated septums or nasal polyps creates a breeding ground. Inhaled foreign bodies (like a peanut lodged in a bronchus) can cause recurring pneumonia in one lung.
And don’t forget secondary causes. Medications like long-term steroids or chemotherapy can lower immunity. Autoimmune diseases like lupus or rheumatoid arthritis can cause low immunoglobulins. Certain cancers, especially lymphomas, can mimic immunodeficiency. In fact, up to 30% of adults diagnosed with CVID later turn out to have another condition hiding behind the low antibody levels.
This is why doctors shouldn’t start IVIG (immune globulin therapy) without proof of functional antibody failure. One study found 22% of patients got IVIG unnecessarily - exposing them to risks like headaches, kidney damage, and blood clots - without any real benefit.
What Happens If You Wait Too Long?
Delaying diagnosis isn’t just inconvenient. It’s dangerous.
Children with SCID who aren’t diagnosed before 3.5 months of age have a 31% higher chance of dying. Early diagnosis - through newborn screening - boosts survival to 94%. That’s the difference between a healthy child and a child who spends their first year in isolation, fighting one infection after another.
Even slower-progressing conditions like CVID cause damage over time. Repeated lung infections lead to bronchiectasis - permanent widening of airways that traps mucus and bacteria. Sinus infections scar the tissue. Liver damage from chronic hepatitis can develop from unnoticed viral infections. Growth delays become permanent. The longer you wait, the more damage piles up.
Studies show that when families use the 10-warning-sign checklist, the average time to diagnosis drops from 9.2 years to just 2.1 years. That’s not a small win. That’s life-changing.
What’s New in Testing?
Genetic testing has changed everything. Five years ago, finding the cause of immunodeficiency meant years of guesswork. Now, next-generation sequencing panels like StrataID Immune test 484 immune-related genes in one go. They find the culprit mutation in 35% of suspected cases - nearly double the old rate.
And it’s getting faster. The NIH is running a 5,000-patient study to build AI tools that predict immunodeficiency from routine blood work. Early results? 92% accuracy. Within five years, whole exome sequencing may be the first test - not the last.
But here’s the catch: these tools are expensive and not available everywhere. In low- and middle-income countries, many people still can’t get basic IgG testing. The World Health Organization is now adding flow cytometry to its Essential Diagnostics List to help bridge that gap.
What Should You Do If You Suspect Immunodeficiency?
Don’t wait. Don’t assume it’s "just allergies" or "a weak immune system." Write down:
- How many infections in the last year
- Where they occurred (ears, lungs, skin, sinuses)
- How long antibiotics were used and if they worked
- Any unusual organisms (fungi, rare bacteria)
- Family history of early deaths or immune problems
- Any growth delays or chronic diarrhea
Take this list to your doctor. Ask: "Could this be an immunodeficiency? Can we check IgG, IgA, IgM, and do a vaccine response test?"
If your doctor says no - or doesn’t know - ask for a referral to an immunologist. This isn’t a specialist you see for allergies or asthma. This is someone who understands immune cell counts, vaccine responses, and genetic testing. They’re the only ones who can give you a real answer.
Recurrent infections aren’t normal. They’re a cry from your body saying something’s broken. And if you listen - and act - you can stop the damage before it’s permanent.



Man, I wish I’d known this when my niece kept getting pneumonia every winter. We thought she was just "sickly" - turns out her IgG was half what it should’ve been for her age. Took two years and three doctors before someone finally ran the vaccine response test. Now she’s on IVIG and thriving. Don’t wait. Write down the symptoms. Bring the checklist. It’s not paranoia - it’s parenting.
Also, the part about CF and foreign bodies? Huge. My cousin’s kid had recurrent right-lung infections for a year. Turned out it was a peanut lodged in the bronchus. No immune issue at all. Always rule out the obvious first.
Thanks for laying this out so clearly.
ok so i just read this and my 4 year old had 6 ear infections last year and 2 sinus ones and i’m like… holy shit am i a bad parent or is this actually a thing??
also she got thrush at 18 months and i thought it was just from the antibiotics but now i’m scared. should i panic? or just call the doc? i’m not even sure what kind of doc to call. pls help.
This is an exceptionally well-structured and clinically accurate summary. The emphasis on age-adjusted immunoglobulin ranges is critical - too many primary care providers still use adult norms for pediatric patients, leading to underdiagnosis.
The vaccine response test remains the gold standard, and its omission is one of the most common diagnostic errors. I’ve seen patients referred for IVIG who had normal IgG levels but zero antibody production post-vaccination. They were mislabeled as "immunodeficient" when the real issue was a failure of B-cell memory.
Also, the point about CF and anatomical causes is spot-on. I’ve had patients with recurrent bronchitis who turned out to have undiagnosed tracheomalacia. Always image before you immunize.
Thank you for highlighting the 9.2-year to 2.1-year diagnosis gap. That’s a public health crisis waiting to be solved.
Oh great. So now we’re diagnosing immunodeficiency because kids get colds? Next they’ll say your kid has cancer because they sneezed during a snowstorm.
Meanwhile, in the real world, we’ve got parents giving their kids vitamin C gummies and calling it a "boost." Meanwhile, the CDC’s got a new flu shot every year and nobody’s getting tested for "dumb immune system."
Also, why is this even a thing? Are we just trying to sell more IVIG? Because I’ve seen the price tag. $10,000 a month? That’s not medicine - that’s a Ponzi scheme with needles.
lol so if your kid gets a cold in october now you’re supposed to assume it’s SCID? i’m sure the pediatrician is just chomping at the bit to run flow cytometry on every 3-year-old with a runny nose.
also i have a 12 year old who’s had 2 pneumonias and he’s a total athlete. he’s got the immune system of a tank. but hey, let’s just test his igg and waste 6 months and $5k because some guy on reddit says "it’s not just bad luck."
also why is this even a post? are we trying to scare parents into buying supplements? because i’m buying the book.
My daughter had thrush at 14 months. I thought it was from the bottle. Turns out it was a sign. I didn’t know what to do. I cried for three days. Now she’s 7 and on monthly infusions. I’m so glad I didn’t listen to the pediatrician who said "it’s just allergies."
Also… thank you. I needed this.
It’s funny how we’ve turned medicine into a mystery box. We’ve got kids with recurrent infections, and instead of asking "why is this happening?" we just throw tests at it like confetti.
But here’s the deeper question: why are we so afraid of a child getting sick? Is it because we’ve been sold the myth that health is the absence of infection? That’s not immunity - that’s control. The immune system isn’t a firewall. It’s a conversation. And sometimes, the conversation gets loud.
Maybe the real red flag isn’t the infections - it’s the panic that follows them.
Still… the checklist? Good. Necessary. Just don’t mistake it for a cure.
Oh wow. So now we’re diagnosing "immunodeficiency" based on a checklist that reads like a horror movie script? Four ear infections? That’s not a red flag - that’s a parenting fail. My kid got 11 ear infections by age 4 and he’s now a varsity wrestler. He didn’t need IVIG - he needed a nap and a warm bath.
And let’s talk about this "vaccine response test." Who the hell is giving a tetanus shot just to check if your kid’s immune system is "working"? That’s not medicine - that’s performance art. You want to test immunity? Let them catch a cold. That’s the original diagnostic tool.
Also, next they’ll say if your kid sneezes twice in a week, they’ve got X-linked agammaglobulinemia. Get real. We’re turning pediatric medicine into a cult of overtesting.
My brother died at 22 from a fungal infection. No one knew why. He was healthy. No diabetes. No meds. Just… kept getting sick. We didn’t know about CVID back then. No one did. Now I look at my nephew’s rashes and I think… could it be? I’m scared to ask. What if I’m wrong? What if I’m right?
This post… it gave me chills. Thank you.
My cousin’s kid got diagnosed with CVID at 5. She was always tired, never gained weight. Doctors called her "picky" and "slow." Then one day, she got pneumocystis pneumonia. That’s when they knew.
Now she’s on monthly infusions. She’s in 3rd grade. She loves dinosaurs. She’s alive.
Just… please. If you’re reading this and your kid’s had 4 ear infections and a thrush patch? Go. Get tested. Don’t wait for the pneumonia.
Just wanted to add something the article didn’t mention - and it’s huge: gut health. A lot of these kids with low IgA have chronic diarrhea or constipation. The gut’s the largest immune organ. If the microbiome’s shot, your antibodies won’t work right.
One patient I worked with had normal IgG levels but zero secretory IgA in stool. Turned out she had SIBO and Candida overgrowth. After 6 months of probiotics and diet changes, her IgA tripled. She stopped getting sinus infections.
Don’t just test blood. Look at the whole system. And yes - antibiotics wipe out your microbiome. That’s why some kids keep getting infections after every course.
Also - thank you for mentioning the 22% IVIG overuse stat. That’s criminal. We’re treating symptoms, not causes.
Okay, I get that this is important, but… how many of these kids are just being overmedicated? I mean, really. How many parents are Googling "recurrent infections" and then dragging their kid to the ER for a CBC because they had a cold in January?
And what about the cost? IVIG isn’t just expensive - it’s invasive. And the side effects? Headaches, kidney damage, blood clots - all from a treatment that might not even be needed.
Look, I’m not saying we ignore the signs. But we’re creating a generation of kids who think they’re broken because they got sick three times last year. Maybe the problem isn’t their immune system… maybe it’s our obsession with perfect health.
Also, I’ve seen kids on IVIG who still get pneumonia. So what’s the point? Just… food for thought.
Just saw the comment about gut health - absolutely right. IgA is produced in the gut mucosa. Low IgA often correlates with dysbiosis, not just primary immunodeficiency.
Also, I’ve seen kids with CVID who improved dramatically with probiotics and vitamin D repletion - not because it cured the disease, but because it reduced secondary inflammation. The immune system isn’t just about antibodies. It’s a network.
And yes - IVIG isn’t a magic bullet. It’s a bridge. The goal is to prevent damage while we find the root cause - whether it’s genetic, environmental, or both.
Thanks for the reminder. We’re not just treating numbers on a lab report. We’re protecting lives.