Medication Absorption Risk Calculator
How Your Digestive System Affects Medication
This tool estimates how your specific conditions and habits may impact medication absorption based on scientific research from the article. Results help you discuss potential issues with your healthcare provider.
Why Your Oral Medication Might Not Be Working
It’s frustrating when you take your pill exactly as prescribed-same time, same food, same dose-but you don’t feel any better. Maybe your pain isn’t controlled. Your INR keeps swinging. Your thyroid levels stay off. The problem isn’t always that the drug is weak. It’s that your body isn’t absorbing it the way it should.
Oral medications make up 70 to 80% of all prescriptions worldwide. They’re convenient, cheap, and easy to take. But the digestive system wasn’t designed to be a drug delivery pipeline. It’s built to break things down, not let them pass through unchanged. And that’s where things go wrong.
The Digestive System Is a Minefield for Drugs
Your gut isn’t just a tube. It’s a complex, dynamic environment with shifting pH levels, thick mucus layers, and powerful barriers that stop foreign substances from entering your bloodstream. The stomach is acidic-pH around 1.5 to 3.5-which can destroy some drugs before they even leave. But most absorption happens in the small intestine, where the surface area is massive-roughly the size of a tennis court-thanks to millions of tiny finger-like projections called villi and microvilli.
Still, even here, drugs face obstacles. The intestinal lining is lined with tight junctions that keep out toxins and pathogens. Unfortunately, they also block many medications. Then there’s the mucus layer, which can be up to 500 micrometers thick in the stomach and still 10 to 100 micrometers in the small intestine. That’s like trying to swim through syrup.
And then there are the transporters. Proteins like P-glycoprotein sit on the surface of intestinal cells and actively pump drugs back out into the gut lumen. If your drug is a substrate for these pumps, it never even gets a chance to enter your blood. That’s why some drugs, like certain antibiotics or chemotherapy agents, show wildly inconsistent results between patients-even with identical doses.
Food Isn’t Just a Meal-It’s a Drug Modifier
Doctors tell you to take some meds on an empty stomach. Others say take them with food. Why? Because food changes everything.
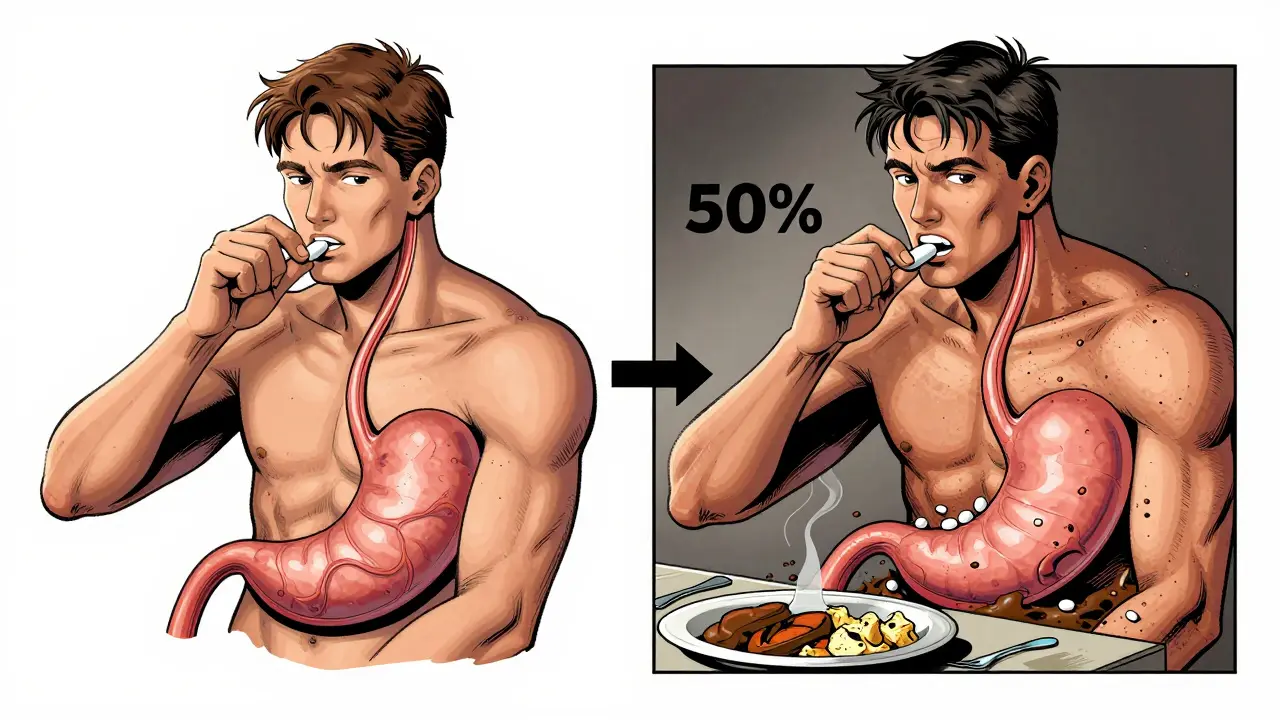
Fatty meals slow down gastric emptying by 2 to 4 hours. That means your pill sits in your stomach longer. For drugs that need quick absorption-like levothyroxine for thyroid replacement-this delay can drop blood levels by 30 to 50%. That’s enough to make you feel tired, gain weight, or crash your mood.
On the flip side, food can help some drugs. Fat-soluble vitamins (A, D, E, K) and certain antibiotics like griseofulvin need dietary fat to dissolve properly. Take them on an empty stomach, and they just pass through. Take them with a meal, and absorption jumps.
Even something as simple as grapefruit juice can mess with your meds. It blocks enzymes in the gut that break down drugs like statins and some blood pressure pills. That means more drug enters your bloodstream than intended-risking toxicity.
Disease Changes Drug Absorption-Dramatically
If you have Crohn’s disease, ulcerative colitis, or short bowel syndrome, your gut isn’t just inflamed-it’s broken. And that breaks how drugs work.
In ulcerative colitis, the inflamed colon can’t absorb drugs like mesalamine properly. Studies show patients with active disease absorb 25 to 40% less of the drug compared to healthy people. That’s why some patients need higher doses or different formulations-like delayed-release pills that target the colon instead of releasing the drug too early.
People with short bowel syndrome have lost so much of their small intestine that even standard doses of antibiotics or vitamins fail. Nurses report some patients need two or three times the normal dose just to reach therapeutic levels. And even then, it’s unpredictable.
Even irritable bowel syndrome (IBS) can delay absorption. If your gut moves too slowly, drugs sit in the upper intestine too long and degrade. If it moves too fast, they zip through before they can be absorbed. The result? Inconsistent effects, erratic symptoms, and frustrated patients.
GLP-1 Drugs Are Changing the Game-And Making Other Meds Less Reliable
Medications like semaglutide (Ozempic, Wegovy) are revolutionizing diabetes and weight loss. But they come with a side effect no one talks about: they slow down your gut.
By delaying gastric emptying and reducing intestinal motility, these drugs can reduce the absorption of other medications by 15 to 30%. That’s a big deal for drugs with narrow therapeutic windows-like warfarin, digoxin, or lithium. One pharmacist on a professional forum described a patient whose INR jumped from 2.1 to 4.8 after starting semaglutide, even though the warfarin dose hadn’t changed. That’s a bleeding risk.
Doctors rarely adjust other meds when starting GLP-1 drugs. Patients aren’t warned. And by the time they end up in the ER with a bruise they can’t explain, the connection is missed.
Formulation Matters More Than You Think
Not all pills are created equal. A tablet and a capsule of the same drug can behave completely differently.
Drugs must dissolve before they can be absorbed. If a tablet dissolves too slowly, it won’t be absorbed fully-especially if it’s moving fast through the gut. That’s why manufacturers tweak the form: salt versions dissolve faster than free-base forms. Crystalline structures matter. Hydrates vs. anhydrates change dissolution rates by 2 to 5 times.
Advanced formulations are helping. Liposomes, nanoparticles, and lipid-based carriers can boost bioavailability by 1.5 to 3.5 times for poorly soluble drugs. Sodium caprate and chitosan can temporarily open tight junctions to let drugs through. These aren’t sci-fi-they’re in use now.
But here’s the catch: most drug labels don’t say which formulation they use, or how it behaves in disease states. You have to dig into clinical studies or ask a pharmacist. Many patients get the same pill year after year, unaware that a generic switch could be changing their absorption.

What Can You Do?
Here’s what actually works in real life:
- Take meds as directed-strictly. If it says “on an empty stomach,” wait 1 hour before eating or 2 hours after. No exceptions.
- Track your symptoms and doses. Keep a simple log: date, time, dose, what you ate, how you felt. Patterns emerge over time.
- Ask your pharmacist about formulation. Not all brands are the same. Ask: “Is this the same as my old pill?” or “Is there a better version for my condition?”
- Speak up if you’re not improving. If your thyroid levels are still off, your pain isn’t controlled, or your INR is wild-say so. It’s not “in your head.” It could be absorption.
- Request a medication review. Especially if you’re on 5+ drugs, have a GI disease, or are over 65. Pharmacists can spot interactions and absorption issues doctors miss.
The Future Is Personalized
Right now, we treat everyone the same. One dose fits all. But your gut is unique. Your transit time, pH levels, mucus thickness, and transporter activity vary from your neighbor’s.
Researchers are testing smart capsules with pH and pressure sensors that send data to your phone. Imagine a pill that tells your doctor: “I dissolved in the jejunum, but your drug didn’t absorb-try a different formulation.”
Companies are building digital models that simulate how a drug behaves in a Crohn’s patient’s gut versus a healthy one. The FDA and EMA are pushing for this. By 2027, 70% of new drugs in development will be large molecules-proteins, peptides, biologics-that can’t be absorbed without help.
The future isn’t just about stronger drugs. It’s about smarter delivery. But until then, understanding absorption issues isn’t optional. It’s the difference between a medication working-and failing silently.
Frequently Asked Questions
Why do some pills work for me but not for my friend, even if we take the same dose?
Everyone’s digestive system is different. Factors like gut motility, pH levels, mucus thickness, and the activity of drug transporters like P-glycoprotein vary between people. Someone with slower transit time or more inflammation may absorb less of the drug. Even minor differences in stomach emptying or diet can change how much medicine enters the bloodstream.
Can food really make my medication useless?
Yes. Fatty meals can delay gastric emptying by 2 to 4 hours, which can reduce peak blood levels of drugs like levothyroxine by 30 to 50%. Some drugs need fat to dissolve-like vitamin D or griseofulvin-so taking them on an empty stomach makes them ineffective. Grapefruit juice can also block enzymes that break down drugs, leading to dangerous buildup.
Why does my doctor keep changing my mesalamine dose?
In ulcerative colitis, inflammation in the colon can reduce how much mesalamine gets absorbed. During flare-ups, you may need a higher dose or a different formulation-like a delayed-release tablet that targets the colon instead of releasing the drug too early. If your symptoms worsen despite the same dose, absorption is likely the issue.
Are generic versions of my GI meds just as good?
They’re supposed to be, but absorption can vary. Generic drugs must meet bioequivalence standards, but those standards don’t always account for disease states like Crohn’s or short bowel syndrome. Some patients report changes in symptoms after switching generics-especially with narrow therapeutic index drugs like warfarin or levothyroxine. Always monitor your response and talk to your pharmacist.
I’m on Ozempic and my blood thinner isn’t working right. Is that possible?
Yes. GLP-1 drugs like semaglutide slow down gut movement, which can reduce absorption of other oral medications by 15 to 30%. This is especially risky for drugs like warfarin, digoxin, or lithium, where small changes in blood levels can cause serious side effects. If you started Ozempic and your INR or symptoms changed, tell your doctor immediately. Your dose may need adjustment.
Should I ask for a special formulation if I have IBD?
Absolutely. Standard tablets may not work if your gut is inflamed or shortened. Delayed-release, enteric-coated, or nanoparticle formulations can help. Ask your doctor or pharmacist if there’s a version designed for inflammatory bowel disease. Some drugs, like Asacol HD, are specifically made to release in the colon-but may not be right if your disease is too advanced.



This is one of those posts that makes you realize how little we're told about what's really happening in our bodies. I've been on levothyroxine for years and never connected my afternoon crashes to eating avocado toast too soon after my pill. Now I wait 90 minutes. Game changer.
Also, the part about GLP-1 drugs slowing absorption? I started semaglutide last year and my INR went from stable to wild. My cardiologist had no idea why. This explains everything.
Grapefruit juice + statins = bad news. Learned that the hard way. 🍊❌
i had no idea food could mess with my meds so bad. i always just took them with my breakfast like everyone says. now im gonna try waiting. thanks for explaining it so simple. this post actually helped me feel less crazy about why i dont feel better even when i do everything right.