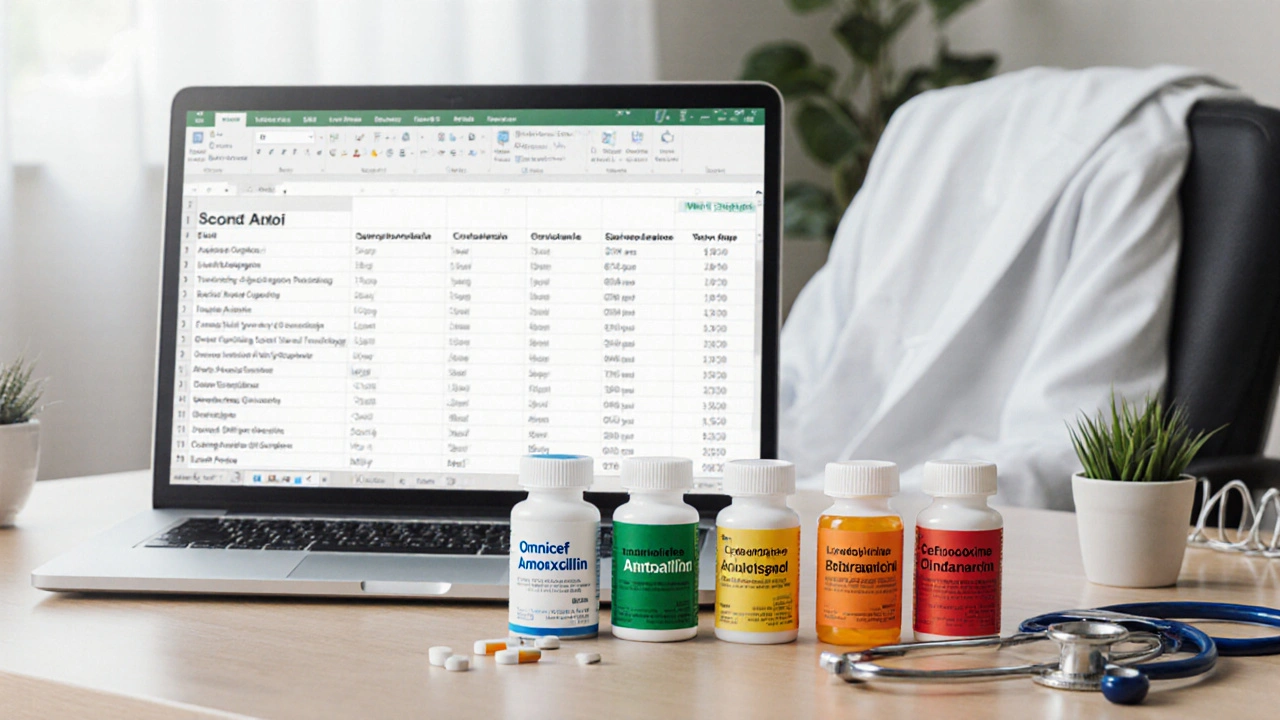
Antibiotic Comparison Tool
Omnicef (Cefdinir)
Class: Third-generation cephalosporin
Uses: Acute otitis media, sinusitis, pharyngitis, skin infections
Frequency: Twice daily
Cost: $30-$45 for 10-day course
Side Effects: GI upset, yellow-green stool, rash
Amoxicillin
Class: Penicillin
Uses: Strep throat, otitis media, pneumonia
Frequency: Three times daily
Cost: $8-$15 for 10-day course
Side Effects: Diarrhea, nausea, allergic rash
Azithromycin
Class: Macrolide
Uses: Community-acquired pneumonia, chlamydia, bronchitis
Frequency: Once daily for 3-5 days
Cost: $20-$35 for 10-day course
Side Effects: Abdominal pain, mild QT prolongation
Cefpodoxime
Class: Third-generation cephalosporin
Uses: Sinusitis, bronchitis, uncomplicated skin infections
Frequency: Once daily
Cost: $40-$55 for 10-day course
Side Effects: Diarrhea, rash, headache
Clindamycin
Class: Lincosamide
Uses: Skin abscesses, dental infections, anaerobic pneumonia
Frequency: Four times daily
Cost: $45-$70 for 10-day course
Side Effects: C. difficile colitis, metallic taste, rash
Comparison Results
When treating bacterial infections, Omnicef is a third‑generation oral cephalosporin (generic name cefdinir) that targets a broad range of gram‑positive and gram‑negative bacteria. It’s often prescribed for ear infections, sinusitis, and skin infections, but many patients wonder if another antibiotic might work better, cost less, or have fewer side effects. This guide breaks down how Omnicef stacks up against the most common alternatives, so you can make an informed choice with your doctor.
Quick Take (TL;DR)
- Omnicef is a broad‑spectrum cephalosporin, effective for many pediatric infections but can cause yellow‑green stool.
- Amoxicillin is cheaper and works well for most upper‑respiratory infections unless the bug is resistant.
- Azithromycin offers a short‑course, three‑day regimen, but resistance is rising for common pathogens.
- Cefpodoxime and cefuroxime are newer cephalosporins with similar coverage but higher price points.
- Clindamycin shines for anaerobic infections but carries a higher risk of C. difficile colitis.
What Makes Omnicef (Cefdinir) Unique?
Omnicef belongs to the cephalosporin family, specifically the third generation. Its key attributes are:
- Spectrum: Covers most streptococci, Haemophilus influenzae, Moraxella catarrhalis, and some gram‑negative rods.
- Dosage form: Available as 125mg, 250mg, and 300mg capsules; also a chewable tablet for kids.
- Pharmacokinetics: Peak plasma levels 1-2hours after ingestion; half‑life around 1.7hours, allowing twice‑daily dosing.
- Safety: Generally well tolerated; most common adverse events are mild GI upset and soft, discolored stools.
Because it isn’t broken down by many beta‑lactamases, it remains active where older penicillins fail, yet it still spares the gut flora better than some broader agents.
Common Alternatives to Omnicef
Below are the top five antibiotics that doctors frequently consider as substitutes. Each entry includes a microdata definition for the first mention.
Amoxicillin is a penicillin‑type antibiotic with a narrow‑to‑moderate spectrum, especially effective against Streptococcus pneumoniae and susceptible Haemophilus species.
Azithromycin is a macrolide that concentrates in tissues, allowing a shorter three‑day regimen for many respiratory infections.
Cefpodoxime is a third‑generation oral cephalosporin with a spectrum similar to cefdinir but a longer half‑life, often dosed once daily.
Cefuroxime is a second‑generation cephalosporin used for sinusitis, otitis media, and some skin infections; it offers a slightly broader gram‑positive coverage.
Clindamycin is a lincosamide antibiotic that targets anaerobes and certain gram‑positive organisms, useful for skin and dental infections.
Side‑by‑Side Comparison
| Antibiotic | Class | Typical Uses | Dosage Frequency | Common Side Effects | Average Cost (US$) for 10‑day course |
|---|---|---|---|---|---|
| Omnicef (Cefdinir) | Third‑gen. cephalosporin | Acute otitis media, sinusitis, pharyngitis, skin infections | Twice daily | GI upset, yellow‑green stool, rash | ≈ $30‑$45 |
| Amoxicillin | Penicillin | Strep throat, otitis media, pneumonia | Three times daily (or BID for extended‑release) | Diarrhea, nausea, allergic rash | ≈ $8‑$15 |
| Azithromycin | Macrolide | Community‑acquired pneumonia, chlamydia, bronchitis | Once daily for 3‑5days | Abdominal pain, mild QT prolongation | ≈ $20‑$35 |
| Cefpodoxime | Third‑gen. cephalosporin | Sinusitis, bronchitis, uncomplicated skin infections | Once daily | Diarrhea, rash, headache | ≈ $40‑$55 |
| Cefuroxime | Second‑gen. cephalosporin | Sinusitis, otitis media, early‑stage pneumonia | Twice daily | Nausea, dyspepsia, mild liver enzyme rise | ≈ $35‑$50 |
| Clindamycin | Lincosamide | Skin abscesses, dental infections, anaerobic pneumonia | Four times daily | C.difficile colitis, metallic taste, rash | ≈ $45‑$70 |

How to Choose the Right Antibiotic
Doctors weigh several factors when swapping one drug for another:
- Pathogen susceptibility: If lab tests show a beta‑lactamase‑producing organism, cefdinir or another third‑gen. cephalosporin often wins over amoxicillin.
- Patient age and weight: Omnicef’s chewable form makes it pediatric‑friendly; clindamycin’s frequent dosing can be hard for kids.
- Allergy history: Penicillin‑allergic patients may need a cephalosporin (if no cross‑reaction) or a macrolide.
- Drug interactions: Azithromycin can boost levels of certain heart medications; clindamycin interferes with neuromuscular blockers.
- Convenience: A once‑daily cefpodoxime dose beats Omnicef’s twice‑daily schedule for patients who struggle with adherence.
- Cost & insurance: Amoxicillin is the most affordable; if insurance covers a brand‑name cephalosporin, the price gap shrinks.
Discuss these points with your prescriber; they’ll match the infection type, local resistance patterns, and your personal health profile.
Safety Profile & Common Side Effects
All antibiotics carry some risk. Here’s what to expect with the six drugs covered:
- Omnicef: Yellow‑green or orange stool is harmless but can alarm patients. Rarely, it triggers a mild rash.
- Amoxicillin: The classic allergic reaction (hives, swelling) is the main concern. Diarrhea occurs in up to 10% of users.
- Azithromycin: Most people tolerate it well; a small percentage experience abdominal cramps or transient QT changes.
- Cefpodoxime & Cefuroxime: Similar GI upset to Omnicef, plus occasional headache.
- Clindamycin: Known for causing C.difficile infection-a serious colitis. Patients should watch for watery, foul‑smelling stool.
If you notice severe rash, breathing difficulty, or persistent diarrhea, contact a healthcare provider promptly.
Cost & Insurance Considerations in 2025
Prescription prices have risen modestly over the past year. Generic cefdinir (Omnicef) typically costs $3‑$4 per 300mg capsule, while brand‑name versions sit near $6 per pill. Most U.S. pharmacy benefit managers place cefdinir in Tier2, meaning a modest co‑pay for insured patients.
Amoxicillin remains the cheapest, often fully covered with a $0‑$5 co‑pay. Azithromycin, especially the extended‑release tablets, sit in Tier2‑3, leading to $10‑$20 out‑of‑pocket. Newer agents like cefpodoxime can be pricier, especially if the brand version is prescribed.
When cost is a big factor, ask your pharmacist about generic swaps or coupon programs. Many chain pharmacies offer a $5‑$10 discount on a 10‑day course of cefdinir.
Real‑World Scenarios
Scenario 1 - Child with acute otitis media: The pediatrician orders Omnicef because the child is allergic to penicillin. The twice‑daily schedule fits the family’s routine, and the chewable formulation ensures the child actually takes the medicine.
Scenario 2 - Adult with community‑acquired pneumonia: Local resistance data shows a high rate of macrolide‑resistant Streptococcus pneumoniae. The physician chooses cefdinir over azithromycin to avoid treatment failure.
Scenario 3 - Patient with a history of C.difficile: Clindamycin is avoided despite its activity against anaerobes; instead, a cephalosporin with a safer gut profile (e.g., cefdinir) is selected.
Key Takeaways
- Omnicef offers broad coverage with a convenient twice‑daily schedule, but its stool discoloration can be unsettling.
- Amoxicillin remains the go‑to for uncomplicated infections where the pathogen is susceptible and the patient isn’t allergic.
- Azithromycin’s short course is attractive, yet rising resistance limits its effectiveness for common respiratory bugs.
- Newer cephalosporins (cefpodoxime, cefuroxime) match Omnicef’s spectrum while offering different dosing schedules and price points.
- Clindamycin is a specialist’s tool for anaerobic infections, used carefully because of C.difficile risk.
Frequently Asked Questions
Can I take Omnicef if I’m allergic to penicillin?
Most people with a true penicillin allergy can safely use cefdinir, as cross‑reactivity is low (<5%). However, you should tell your doctor about the severity of your allergy. If you’ve had an anaphylactic reaction, the clinician may opt for a non‑β‑lactam alternative like azithromycin.
Why does Omnicef turn my stool orange?
The orange or yellow‑green color comes from unabsorbed cefdinir that binds to iron in the gut. It’s harmless and disappears after the course ends. If you’re concerned, try taking the pill with a full glass of water and avoid iron‑rich foods during the treatment.
Is a 5‑day course of Omnicef as effective as a 10‑day course?
Clinical trials show that a 5‑day regimen (300mg twice daily) is non‑inferior for mild to moderate otitis media and sinusitis. For deeper infections like osteomyelitis, a longer 10‑day course is still recommended.
How does the cost of Omnicef compare to generic amoxicillin?
Generic amoxicillin averages $0.30‑$0.50 per 500mg tablet, making a 10‑day course under $5. Generic cefdinir is roughly $1‑$1.50 per 300mg capsule, so a comparable 10‑day course costs $30‑$45. Insurance coverage can narrow this gap, but amoxicillin remains the cheaper option.
When should I pick azithromycin over Omnicef?
Azithromycin shines when a short, once‑daily regimen is needed-such as in travelers who may miss doses, or in patients with gastrointestinal intolerance to cephalosporins. It’s also the drug of choice for atypical pathogens like Mycoplasma pneumoniae.


I think it’s useful to look at the big picture when choosing an antibiotic. Omnicef gives you solid coverage for both gram‑positive and gram‑negative bugs, which is why it’s a common go‑to for kids with ear infections. Compared with amoxicillin, it’s a bit pricier, but the twice‑daily dosing can be easier for families than a three‑times‑daily schedule. On the downside, that yellow‑green stool can scare patients, even though it’s harmless. If cost is a major factor, the cheap generic amoxicillin is still a great first‑line option for susceptible organisms. Bottom line: match the drug to the bug, the patient’s allergy profile, and the wallet.
If you can’t afford Amoxicillin, you’re probably better off with Omnicef.
One must consider the hidden agenda behind pharmaceutical pricing, as large corporations subtly steer prescribing habits toward more expensive branded equivalents. The data presented in the comparison chart conveniently omits the long‑term ecological impact of broad‑spectrum agents such as cefdinir, thereby shielding the reader from inconvenient truths. Moreover, the mention of “average cost” fails to account for regional insurance disparities that are often manipulated for profit. In light of these observations, a cautious clinician should critically evaluate whether the marginal benefit truly outweighs the covert economic incentives.
Let’s cut through the hype and call a spade a spade: Omnicef isn’t the miracle drug some marketing teams want you to believe. First, the claim that it “covers most gram‑positive and gram‑negative bacteria” is technically true, but it also means you’re hammering the microbiome with a broad‑spectrum weapon when a narrow‑spectrum penicillin would suffice. Second, the twice‑daily schedule is heralded as convenient, yet many patients forget the second dose, leading to sub‑therapeutic levels and resistance. Third, the “yellow‑green stool” side effect-while harmless-creates a needless alarm that drives patients to the ER for reassurance, inflating healthcare costs. Fourth, the price point of $30‑$45 is nothing compared to the $8‑$15 you’d pay for amoxicillin, especially when insurance co‑pays are similar. Fifth, the comparison completely sidesteps the issue of beta‑lactamase‑producing organisms that can render cefdinir ineffective in areas with high resistance. Sixth, the table pretends that side‑effect profiles are equal, ignoring the documented higher incidence of rash with cephalosporins in certain ethnic groups. Seventh, you’ll find that cefdinir’s bioavailability is lower than amoxicillin, meaning you need a higher dose to achieve the same plasma concentrations. Eighth, the once‑daily alternatives like cefpodoxime actually improve adherence for patients with busy schedules. Ninth, the claim that Omnicef spares gut flora better than clindamycin is a stretch, as any beta‑lactam will disrupt the intestinal microbiome to some degree. Tenth, the reliance on “average cost” masks the fact that many pharmacies charge premium prices for the brand name version. Eleventh, the article never mentions the potential for drug‑drug interactions with calcium‑containing antacids, which can reduce cefdinir absorption. Twelfth, in pediatric cases, the chewable tablet is often too sweet, leading to over‑consumption and dosing errors. Thirteenth, the “broad coverage” argument ignores the fact that overuse of broad‑spectrum antibiotics fuels the global antimicrobial resistance crisis. Fourteenth, the piece glosses over the fact that azithromycin’s short course can be a game‑changer for compliance, despite rising resistance. Fifteenth, before you hand out Omnicef, ask yourself if you’re truly treating an infection or simply appeasing a parent’s demand for a “strong” medicine.
Dear readers, the choice between Omnicef and its alternatives can feel overwhelming, but a systematic approach helps 😊. Consider the infection type, any known drug allergies, and the cost burden on the patient. For a straightforward ear infection in a child who is penicillin‑tolerant, amoxicillin remains economical and effective. If the pathogen is β‑lactamase‑producing, cefdinir’s stability offers an advantage, albeit at a higher price. Always discuss insurance coverage and possible coupon programs to lessen out‑of‑pocket expenses. Stay informed and stay healthy! 👍
From a pharmacokinetic standpoint, cefdinir exhibits a moderate volume of distribution (Vd ≈ 0.2 L/kg) and a half‑life approximating 1.7 h, necessitating BID administration to maintain plasma concentrations above the MIC for target pathogens. Its molecular architecture, featuring a 7‑acetoxy group, confers resistance to many class A β‑lactamases, thereby preserving activity against β‑lactamase‑producing strains where amoxicillin fails. However, the drug’s oral bioavailability (~55 %) is suboptimal relative to penicillins, implicating dose escalation strategies in pharmacodynamic modeling. Moreover, the facultative alteration of gut microbiota composition post‑therapy has been documented via 16S rRNA sequencing, underscoring the importance of probiotic adjuncts. In contrast, azithromycin’s extensive tissue penetration (tissue:plasma ratio >10) and prolonged post‑antibiotic effect facilitate a truncated dosing regimen, albeit with a distinct resistance selection pressure on macrolide‑susceptible organisms.
Omnicef works well for many infections, but it does cost more than amoxicillin and can turn stools a bright color, which can worry patients. If the bug is known to be sensitive to penicillin, the cheaper option is usually best. Remember to check for any penicillin allergy before switching. The twice‑daily schedule is easy for most people to follow.
Hey folks, just wanted to throw in a quick encouragement note for anyone wrestling with the antibiotic decision. It’s easy to get lost in the tables and price tags, but think of it like picking the right tool for a repair job-you wouldn’t use a hammer to tighten a screw, right? Match the drug to the infection, consider the patient’s age and any allergies, and don’t forget to factor in how easy the dosing schedule is for them to stick with. If cost is a concern, talk to the pharmacist about generic options or discount cards; they’re often a lifesaver. And remember, the best antibiotic is the one that actually clears the infection without causing extra trouble. You’ve got this!
While your pep‑talk is heartfelt, let’s not sugar‑coat the reality that many clinicians still default to the cheapest drug without weighing the microbiological nuances, which leads to suboptimal outcomes. The “one‑size‑fits‑all” mentality you promote can inadvertently encourage antibiotic overuse, fueling resistance in ways that the average patient never sees coming. It’s not enough to say “match the drug to the infection” when the infection profile is often obscured by delayed cultures and empirical prescribing. Moreover, relying on pharmacists for discount cards is a short‑term fix that ignores the systemic pricing disparities built into the healthcare market. If we truly want to improve stewardship, we need to push for rapid diagnostic tools and clinician education, not just feel‑good slogans.
Bottom line: pick the cheapest effective drug, but don’t sacrifice safety. If you’re allergic to penicillin, go with cefdinir or azithro. Talk to your doc and get the right prescription.
Quick tip: when you get the prescription, ask the pharmacist if a generic version is available-it can shave off a lot of cost. Also, double‑check the dosing schedule; missing a dose can turn a good treatment into a failure.
In the vast tapestry of microbial warfare, each antibiotic is a brushstroke, painting the outcome of health or disease. Omnicef adds a bold splash of broad‑spectrum vigor, yet it risks drowning the delicate flora in its wake. Sometimes the subtle hue of amoxicillin is enough to bring harmony, while the fiery dash of azithromycin can scorch resistance patterns if misused. The artist must choose his palette wisely, guided by both science and the patient’s story.
Omnicef: good for beta‑lactamase producers. Amoxicillin: cheap, first line. Azithromycin: short course, watch for QT. Cefpodoxime: once daily, higher cost. Clindamycin: anaerobes, C. difficile risk.
The drama of choosing an antibiotic mirrors the tragedy of a Shakespearean hero-torn between duty and desire. Omnicef stands as the valiant knight, brave yet costly, while amoxicillin whispers promises of simplicity. Yet the villain, resistance, lurks in the shadows, ready to strike any misstep. Choose wisely, lest the plot twist be a relapse.